If you take insulin to manage your diabetes, you could be taking anywhere from 1 to 10 injections per day.
And where you inject your insulin matters — not only because certain areas of the body are more ideal than others, but also because it’s important to use a variety of areas.
In this article, we’ll discuss everything you need to know about insulin injection sites.
Table of Contents
- Why it matters where you inject your insulin
- What are the best injection sites for insulin?
- Why you should rotate your insulin injections
- How I rotate my insulin injection sites
- Lipodystrophy: a side-effect of not rotating injection sites
- Never inject two types of insulin in the same area at the same time
- Can you inject insulin into muscle?
- Proper and safe insulin injection technique
Why it matters where you inject your insulin
Insulin is designed to be injected (or delivered via an insulin pump) into body fat — also known as “subcutaneous tissue.”
The rate at which your insulin is absorbed is largely based on the assumption that it’s being injected into fat, rather than muscle.
When a pharmaceutical company tells you that the “onset” of your Novolog or Humalog insulin is 15 minutes, for example, that is based on when it is injected into body fat. The “peak” of its efficacy and the “duration” of it staying in your bloodstream are also dependent on it being injected into body fat — not muscle.
What are the best injection sites for insulin?
The best injection sites for insulin are a variety of locations on your body that are both easy to reach and contain adequate body fat. (The leaner you are, the more you may need to “pinch” your layer of fat in order to avoid injecting into muscle.
- Belly fat
- Side-torso fat (“love handle” area)
- Lower back fat
- Thigh fat (on the outer or inner sides of your leg)
- Butt fat (upper, middle, sides, etc.)
- Arm (back or sides)
These areas are the most likely to have enough body fat to comfortably inject insulin into using a pen or syringe.
Why you should rotate your insulin injections
Every time you inject insulin into a certain area of your body, that location of skin and body fat is “injured” and has to heal. Over the course of years injecting insulin into your body, scar tissue will develop.
You may not see evidence of that scar-tissue on the outside of your body, but it’s there on the inside.
The more you inject insulin into the back of your arm, the more scar tissue will develop there. As people with diabetes, it’s very easy to get into the habit of injecting into the same spot over and over because it’s easy to reach and comfortable to access in the middle of a restaurant, for example.
But scar tissue will significantly affect your body’s ability to absorb the insulin from that last injection, and you could end up needing more insulin to do the same job even though your insulin needs didn’t change. Instead, it’s just scar-tissue built-up and interfering with the absorption of your insulin dose.
Rotating your injection sites is critical.
- If you used your left arm for your lunchtime injection, you should use your right arm for your dinnertime injection.
- If you used the left side of your bum for your long-acting insulin injection last night, you should use your right side for tonight’s injection.
The more you can rotate the areas of your body and the exact spots on each area, the less scar-tissue will build-up and the more easily your body will absorb that insulin.
How I rotate my insulin injection sites
While I use my abdomen and arms for my rapid-acting injections, I use my glutes and lower back for all of my basal (long-acting insulin) injections.
I have a very home-made but also very effective way of keeping track of my injections so I remember to rotate them.
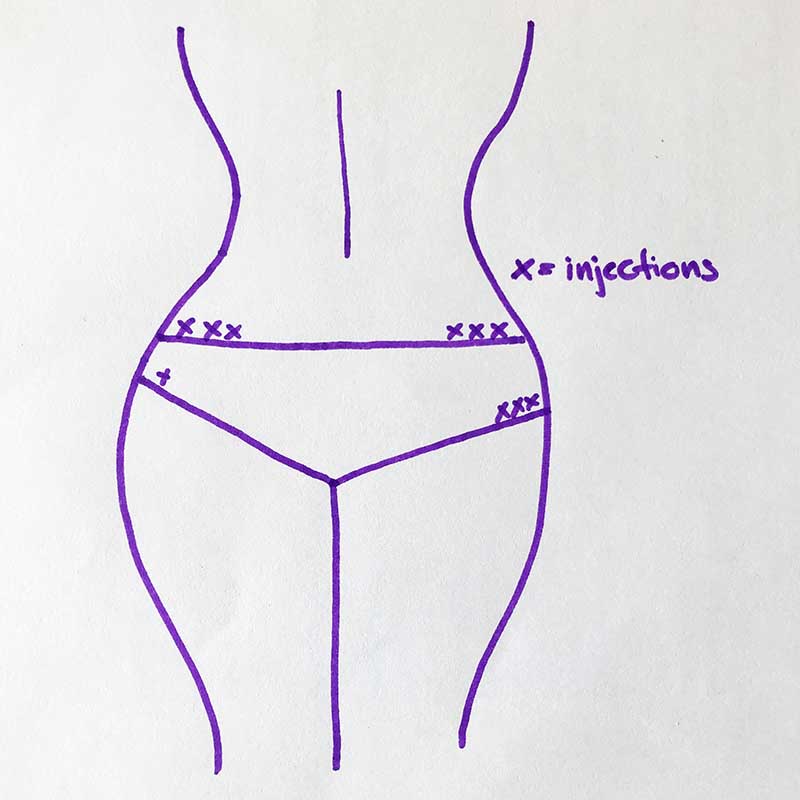
To make sure that I do proper injection rotation, I have a piece of paper where I note down my injections (see image below). I usually switch from right to left side daily and will start with injecting right above the bikini line, then switch to below the bikini line, and lastly inject alongside the bikini line.
This rotation pattern takes me about a month to get through before I start all over again. So far, that has worked really well for me. I have no lumps and my insulin absorption is still really good after 20 years with diabetes.
Lipodystrophy: a side-effect of not rotating injection sites
Lipodystrophy (LD) is a condition affecting body fat tissue and it’s very common in people who take multiple daily insulin injections. Other variations include “lipohypertrophy” (LH) or “lipoatrophy” (LA). All of which concern damage, scar-tissue or hard lumps in the fatty tissue where you’ve been injecting insulin.
The best way to prevent LD from developing in your own skin tissue is by making sure you rotate your inject sites and aren’t repeatedly injecting insulin into the exact same area of tissue.
If you already have signs of LD, you can talk to your primary care and ask for a referral to a dermatologist for further guidance on reducing it.
Never inject two types of insulin in the same area at the same time
You should also keep in mind that you do not want to inject two different types of insulin in the same area at the same time.
If you’re taking a long-acting insulin dose and a rapid-acting insulin dose at 7 a.m., you should make sure they are injected into two completely different areas of your body.
Some insulins can affect the potency, absorption, and efficacy of other insulins if they “meet” each other in that subcutaneous tissue.
Can you inject insulin into muscle?
The short answer is yes, but you shouldn’t inject insulin into muscle unless it’s very intentional and you understand the consequences and risks.
Injecting insulin directly into muscle is going to completely change how quickly it is absorbed into your bloodstream and how it quickly it starts affecting your blood sugar levels.
The “onset,” “peak,” and “duration” will all change when insulin is injected directly into muscle tissue.
(It’s also going to be a bit more painful!)
Never inject long-acting insulin into muscle.
Long-acting insulin (Tresiba, Lantus, Toujeo, Basalgar, NPH, Levemir) needs to stay active in your body for the intended duration of time. Injecting into muscle means it’s going to be out of your bloodstream far sooner and thus put you at a high-risk for severely high blood sugars and diabetic ketoacidosis (DKA).
Consider injecting rapid-acting insulin into muscle if…
When treating a high blood sugar with a correction dose of insulin, the amount of insulin you use needs to be finely tuned to ensure your blood sugar doesn’t severely plummet.
The goal is to bring your blood sugar back down into a safe range — that requires an accurate “correction factor” and some patience.
You can consider injecting insulin into muscle if:
- Your blood sugar is extremely high, over 250 mg/dL. Injecting your correction dose of insulin into muscle could help it come down sooner.
- Your insulin pump failed and you need to get insulin active in your system as quickly as possible.
- You’re combating sudden severe stress that is going to (or has already) spiked your blood sugar.
- You take steroids for a condition like Addison’s disease. Consider injecting the insulin dose you use to compensate for that steroid dose into muscle.
- Your blood sugar is high because you’re severely dehydrated and potentially producing ketones.
- Your blood sugar is high prior to an important activity that calls for a lower blood sugar level (like an athletic event or surgery).
- You forgot to take insulin with your meal. Injecting directly into muscle can help get the insulin on-board sooner and prevent that post-meal spike.
Keep in mind that you should always talk to your doctor prior to making changes in how you take your insulin.
Proper and safe insulin injection technique
Well, this is simple. Every time you inject insulin into body fat or muscle, it’s important to ensure that the area is clean and that you are using a clean syringe or insulin pen.
Insulin syringes and pen needles are designed to be used once.
And you should sanitize the intended injection site with an alcohol swab before every injection.
Is this realistically always possible? Not really — not in the real life of diabetes when you’re taking many injections a day. But the goal is to inject insulin into the cleanest location possible to prevent infections.
Having to inject insulin into your body on a daily basis is not fun, but it keeps us alive. The more thought and consideration you put into where you inject your insulin, the better off you’ll be.
Suggested next post: How to improve your insulin sensitivity
If you found this guide to insulin injection sites useful, please sign up for our newsletter (and get a sign-up bonus) using the form below. We send out a weekly newsletter with the latest posts and recipes from Diabetes Strong.





“kissy”
Thanks for the information about site rotation I have gotten a few hard lumps but I am starting your rotation suggestion today.
Ken Messenger
Hi, I’ve had Type 1 diabetes since my pancreas ruptured in 1997. I started with MDI but my
endocrinologist suggested I try the Medtronic insulin pump. I’m 80 years old now and have never had the kinds of issues you discuss with varying activity levels. Perhaps your basal settings were too high. I don’t have a CGM so I depend upon my knowledge of insulin and diabetes (I retired 10 years ago as a Registered Nurse) plus experience using the pump. It is not rocket science. I respect your perspective and realize it is likely to be helpful to many people but I’m writing this because I fear it may deny some the benefits of todays intelligent insulin pump therapy. Thanks for letting me add my $0.42 (inflation you know).
RJ
Hi. My 12y/o daughter is type 1 for 6 years. She’s going through a tough time with all the changes in her body. It’s wreaking havoc on her BG and it’s all taking a toll on her emotionally. Is their anyway you could help young type 1 girls like her (and their parents) navigate through this tough time in their lives. Would love to hear your thoughts. Perhaps write an article about it. I know that my daughter has no one in her life that has gone through what she is going through. So someone like yourself could be a tremendous source of inspiration to her. Thanks.
Christel Oerum
I wish I could be a better resource when it comes to kids and diabetes. I was diagnosed when I was 19 years old, so I can’t give a personal perspective on how it is to be a teenager with diabetes. That’s also one of the reasons why you at this time mainly see articles written with adults in mind on Diabetes Strong. But that doesn’t mean that we shouldn’t consider it.
For now, though you and your daughter might find the support you need through Beyond Type 1 or one of the many Facebook groups for parents. I also think the Juicebox podcast would be a great resource for both of you
Gypsy
It can be difficult to keep in the range you are looking for, I have been a type 1 for 38.5 yrs. The best advice I have is to keep a good schedule. It helps your body cope with the changes happening. Another option is an insulin pump but that can get expensive. If you need someone to talk to email me.
Regis McKenna
I became a type 1 diabetic when I was 19 and, for me that was an advantage. My older brothers became a diabetic when he was 10 years old. That was in 1945. He struggled his whole life because he really didn’t pay much attention to his diet and social pressures on young diabetic only increases as they move into their teens. At 19, I could look at my brother and see what not to do. Diabetes was a rare disease in the 1940’s and their were few specialist to help.
This month I have been a diabetic for 64 years.
What to do?
1. Buy a Dexcom sensor.
2. If possible use an insulin pump that is comparable withe Dexcom. Dexcom checks your blood sugar every 15 minutes and records the data sent to a pump or iPhone.
3. Take up sports. I ran for over 50 years and still use a spin bike for an hour every day. Exercise is vital to keeping your bold tissue healthy for good insulin absorption.
4. Stick to a eating program. I don’t call it a diet, I like what I eat but I eat pretty much the same thing everyday. Avoid pure sugars, candy, but find foods you like and add to meals. I eat salmon almost every evening for dinner and I love it. Cup of yogurt with some papaya or mango is also good for breakfast. 5, Don’t worry or get upset if you are not always perfect or your blood A1C is not what it should be. Just make a new commitment to get better. Always, always stay positive! Attitude has a lot to do with how you address your desires. Stay strong, you have a lot of years ahead of you so plan on enjoying those years by staying healthy.
Cindy Holland
As a new diabetic at 61 your articles have helped me become confident in my insulin therapy. I often was in a panic and often fearful of the unknown and overall becoming depressed. I want to thank you for being so informative in your array of topics; you are my blessing!
Christel Oerum
Cindy, I’m so glad Diabetes Strong has been a good resource for you. A diabetes diagnosis can be so hard. Please know you’re not alone
S Basava kiran
thank you mam valuable info & about injection rotations & techniques very helpful to me mam
S Basava kiran
Thank you so much mam very helpful article helps in knowing info mam about usage of insulin injection techniques. ???
Fikile
I’m a newly diagnosed Type 1 to be specific injecting 4 times a day so I need all the assistance I can get.
Christel Oerum
I’d recommend learning as much as you can about the condition so that you can become as self-managed as possible. This would be a good place to start: https://diabetesstrong.com/category/diabetes/type-1/
Komal Patil
Hi
Christel Oerum
Im from India and Type 1 Diabetic since the age of 9 and currently working as an health educator in a reputed hospital in Mumbai. Can you advice some Free or Paid Certification Online Diabetes Educator Course which will benefit me professionally as well as on personal front
Christel Oerum
I think looking up resources on the Association of Diabetes Care & Education specialists (ADCES.org) is probably your best bet
Juan Noval
Thanks for the concise and clear explanation on how to rotate injection sites. In all my years with T1D I have never heard or read a better rotation plan. I have gotten into the lazy habit of using just my belly fat for both my Humalog and Tresiba injections and I am sure that it is not being absorbed as efficiently by my body as possible. I will implement it starting today to see if I have better results with night time highs. Thx again. =)
Christel Oerum
Glad this was helpful!
Rebecca
What about using your calf? Easy to reach when wearing slacks and discreet as an under the table shot at a restaurant.
Christel Oerum
That would for most be considered a muscle injection. If you’re comfortable doing it and understand that the insulin will most like work faster I don’t see a huge issue