This is a detailed article about what happened when I tried to experiment with a low-fat, high-carb diet led by Cyrus Khambatta from Mastering Diabetes for “ultimate” sensitivity to insulin.
This is a lengthy post because I want to do the experience justice. I also want to give enough detail to give proper credit and acknowledgment to those who do enjoy and thrive while eating a high-carb, low-fat, plant-based diet.
But by Day 9 of this experiment, I’ve realized I’m not one of those people.
Before This Experiment
My “usual” over the past few years has varied between a low-carb diet (50 grams or less of carbs) or a lower-than-average carb diet (100 grams or less). And sprinkled in there are also indulgences like gluten-free pizza or the incredible gluten-free chocolate cake I made for my twin brother when he came to visit or gluten-free Christmas cookies.
My point is: I save my carbs for the good stuff: pizza night, burger night, and occasional homemade desserts. Pizza night is probably 3x a month. Burger night is far rarer, 1x a month at most.
I’ve managed to keep my A1C between 5.5 and 6.5 with this flexible approach to eating mostly whole foods, mostly low-carb, and “saving” room in my “carb budget” for the carbs that I enjoy the most. This also makes blood sugar management around those treats easier because your low-carb choices all day require very little effort and insulin/carb juggling.
You can also keep your carb intake still relatively low if you’re just indulging once per day (or once per week, etc., your choice), so you’re preventing any feeling of deprivation but still eating a mostly lower-carb diet.
I was also a big fan of intermittent fasting prior to this experiment, and I continued to do 16-hour fasts while following Cyrus and Robbie’s program.
My insulin doses before this high-carb experiment
- My Tresiba (basal) dose was 10 units. (Prior to getting Norovirus, my Tresiba dose was at 11 units. But a week of consuming only Gatorade and rice cakes is inevitably going to bring that down.)
- My insulin-to-carb ratio using Humalog was generally 1:12 (1 unit of Humalog for every 12 grams of carbs).
- My correction factor was generally 1:100 (1 unit would reduce my blood sugar by 100 points).
Over the past 10 years: I’ve experimented with high-protein/low-carb plans, ketogenic eating, being pregnant & eating a giant bowl of cereal every day because otherwise my pregnant soul simply could not go on—seriously!
I ate lower carb during pregnancies than the average person, but it was still high-carb for me…and my A1c stayed between 5.1 and 6.1 because of diligent blood sugar checking and expected fine-tuning of insulin doses as pregnancy with type 1 diabetes progresses.
I’m a big, big, big believer that different phases of life call for different shapes of eating.
A sample typical day of low-carb eating, for me, looked like
- Fasting until 12 p.m. or 1 p.m. (Occasionally I would eat as early as 11 a.m. if the toddler and 10-month-old were trying my energy and patience more than usual and I needed fuel ASAP).
- My first meal would be a flaxseed muffin in a mug with butter or peanut butter, OR a big green salad with 2 eggs OR sauteed/air-fried veggies (cabbage, broccoli, onion, carrots, etc.) with 2 eggs.
- My second meal would be an apple & 2 slices of cheese OR carrots & hummus OR homemade eggplant chips with olive oil, paprika & salt (made in the food dehydrator)
- Some days, I would strive to not eat again so that when my husband comes home from work, I could hop on the treadmill for fasted cardio which ensures I would burn fat for fuel rather than glucose if it had been 4 hours or longer since my last meal.
- Or if I was just plain hungry, I might have an Orgain protein shake with unsweetened almond milk & peanut butter (if I hadn’t had peanut butter already that day) OR sauteed tofu with salad OR homemade Psyllium Husk Rolls with butter…(which are awesome for your digestive tract, by the way! And require zero insulin).
- And lastly, dinner would be something as simple as steak and veggies OR low-carb BLTs OR edamame fettuccine with sautéed veggies and homemade meatballs OR a giant salad with (gasp) full-fat commercial salad dressing & a bunless hamburger OR a high-carb indulgent treat of tacos or pizza.
- During the month of March, my discipline in the treats and sweets department was pretty lacking. I ate low-carb during the day but indulged more nights than not in some variety of wine, chocolate, or a high-carb/high-fat dinner like pizza or burgers. That being said, I didn’t gain weight and my insulin needs didn’t change because the rest of my day was still very low-carb and consisted of whole foods.
In some order, which varies, those are my go-to meals lately.
Why I wanted to give High-Carb/Low-Fat a try
I began this high-carb, low-fat experiment on April 1st for a few reasons.
- I was feeling bored and unmotivated by my current eating. While I enjoyed all of those foods, it was very much tried and true and there wasn’t much “experiment” left to it. And I’m a girl who clearly loves to tweak and experiment and see what happens.
- I’ve always respected Cyrus Khambatta’s completely controversial passion for his plant-based high-carb, low-fat approach to thriving with diabetes. I published many of his articles at DiabetesDaily during my 5 years as Editorial Director, and stand by the fact that there is no one-size-fits-all diet for everyone. If you feel best eating beans and strawberries all day, good for you! I don’t need to convince you to eat my way if you’re enjoying eating yours. But hey, if you’re looking for help, I’m happy to share my two cents on what works for me and many of my friends.
- I had just gotten Norovirus (most likely from the local children’s library), and after 5 days of eating nothing but Gatorade and rice cakes, I realized I was perfectly primed to give Cyrus’ approach a shot. He had explained to me earlier that it’s essential to give your body a bit of “transition time” if you were previously eating a lot of fats. Your liver and your muscles are (in layman’s terms) storing a great deal of extra fatty acids, and switching suddenly to high-carb isn’t gonna be pretty if you rush that transition phase.
- I did still want to lose those remaining 10 lbs. And while eating clean and low-carb has always worked well for me in the past (my postpartum weight loss being the most recent case in point), I was ready to be open-minded and experiment with something new.
The “Mastering Diabetes” High-Carb, Low-Fat, Plant-Based Program
In a nutshell, (because if you really want to try it, you should become a member and learn from the experts, not me), Cyrus Khambatta, Ph.D. and Robbie Barbaro teach an approach to diabetes management and nutrition that is the direct opposite of a ketogenic diet.
You should know: Cyrus and Robbie are two of the most upbeat, positive, and passionate nutrition coach fellas you could find. They are 100% dedicated to their mission of teaching people how to achieve healthier lives with diabetes through their program, and that dedication is admirable.
I have a great amount of respect for both of them even if I don’t feel that their program is right for me.
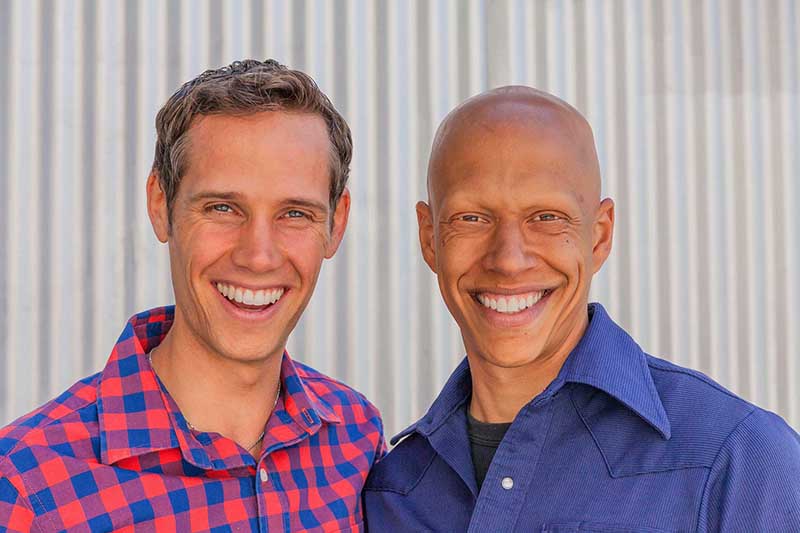
The gist: Achieve ultra-sensitivity to insulin through an extremely low-fat diet that is high in carbohydrates from “plant-based, whole foods.”
Your daily fat intake goal is between 20 to 30 grams of fat. While 30 is considered within the goal, Cyrus emphasized that keeping your fat intake down at 20 grams per day leads to mega-mega changes in insulin sensitivity and insulin resistance.
Confused?
Yes, eating a low-carb diet reduces your need for insulin, but overall, Khambatta and Barbaro teach that it can make you more insulin-resistant because fats “blunt” our sensitivity to insulin.
A ketogenic diet (or low-carb diet) works because even if you are technically more resistant to insulin due to the high-fat intake, your carb intake is low enough that your insulin needs are still plenty low regardless.
If you’ve ever tried this approach, you know that when done properly it makes nearly non-diabetic blood sugar levels practically effortless–taking 1 unit here and there for low-carb meals of protein/fat and veggies.
Cyrus and Robbie, on the other hand, teach folks to severely reduce their fat intake with a goal of 20 to 30 grams total daily, and thus make your insulin needs for large quantities of carbohydrates much lower.
A bowl of bananas and mangos for breakfast? A lunch of beans, corn, spinach, oranges, and berries? A dinner of brown rice and more veggies and more fruit? You bet. Tons of carbs. It took 300 grams easily for me to meet my nutritional needs as a 5’2 female. Easily 600 grams for active males.
A sample day of high-carb eating for me looked like
- Fasting until 1 p.m. (this was harder on this diet, I felt pretty damn hungry by 11 a.m. and waiting impatiently to end the fasting window
- Oat bran with blueberries, salt, and cinnamon
- Homemade 3-bean salad with sautéed veggies (onions, celery, corn)
- Apple, strawberries, and a couple of times I had gluten-free Fig Newtons to treat lows
- Protein shake with unsweetened almond milk
- Black bean pasta with tomato sauce & salad OR potatoes with green beans
Their client testimonials include a variety of type 1 and type 2 diabetics who have reduced their insulin usage, reduced their A1c levels, and are eating 300 to 600 grams of carbs per day. This clearly has worked well for a variety of people.
Like all extreme diets, the question we can never answer for sure is how long people continued to follow this diet (or a keto diet) after a testimonial was written.
Regardless, when you severely reduce any one macronutrient, you’ll need to compensate by drastically raising your consumption of another macronutrient.
- In the bodybuilding world, it’s usually fat that’s decreased. Protein goes up dramatically and carbohydrates are carefully placed for maximum usage for recovery.
- In Khambatta and Barbaro’s approach, fat is severely decreased. Carbohydrate consumption rises dramatically, and your protein consumption is more moderate.
- In the low-carb/ketogenic world, carbohydrate consumption is severely decreased. Fat consumption rises dramatically, and protein consumption is more moderate.
An aspect of their philosophy where I really disagree with Cyrus and Robbie is here: Within their program, you can find a detailed explanation of non-diabetic blood sugar “norms” and A1c goals vs. diabetic blood sugar “norms” and A1c goals.
They argue that non-diabetics have blood sugars fluctuating up to 140 mg/dL regularly. If this were the case, however, non-diabetic A1c levels wouldn’t be in the low 5s and high 4s. This argument, seemed to me, like an attempt to dismiss the issue that carbohydrates do in fact raise blood sugar more than any other food.
While I absolutely believe people with diabetes should strive for A1c levels that feel safe and sustainable to them, there is no denying that an A1c of 6 percent is still much higher than a non-diabetic would see from “perfect” blood sugar levels.
Within the first week of eating high-carb/low-fat: After two or three days, I dropped my 10-unit Tresiba dose down to 9. On Day 3, I went out to dinner with my husband for our anniversary and ate gluten-free pizza, gluten-free beer, and gluten-free cake! It was delicious. But obviously didn’t follow the program at all.
I did a 24-hour intermittent fast that day to help compensate for the extra load of indulgent calories, carbs, and fat. But it was delicious and worth every unit of insulin.
By the next morning, I was back to business and ate following the program: loads of veggies, some grains, no added oils (even in salad), and fruit. And potatoes!
I could definitely feel my body burning through the food I was eating. And to be honest, food was all I could think about during my non-fasting window of about 1 p.m. until bedtime. As Cyrus warned me, when you’re eating this way, it takes a lot more calories and larger quantities of food to feel full and get what you need.
“If you’re hungry, eat,” he encouraged. And I was. Very.
By Day 5: Eating oat bran (rather than oatmeal) was starting to give me that same lethargic feeling that oatmeal and rice have given me in the past. I just don’t feel good when I eat those foods. It’s more extreme with the oatmeal but I was feeling it with the oat bran, too. My body is not fond of grain. Even in a low-fat diet.
I did notice that when I did need to correct a high blood sugar, it came down much more quickly than when I was eating a diet lower in carbs. With so little fat in my diet, my insulin worked much more quickly in my system and affected my blood sugar much more quickly, too.
By Day 6: I had lost 1 pound according to the scale. I was feeling some momentum, and I clearly hadn’t even done it 100%. I was also enjoying the challenge of minimal fat intake.
But I should add that I’ve never been a “gassy” person and holy moly, the daily bean intake was making me extremely gassy. I eat a lot of fiber in my usual diet, so my digestive tract is plenty accustomed to high-fiber intake, but the beans are another story.
And this gassiness continued on every day. It also made me feel surprisingly constipated — something else I’d never felt on my usual nutrition plan.
By Day 7: Despite seeing clear evidence of mega insulin sensitivity, this is when things started to unravel a bit, including my enthusiasm.
My insulin doses after 1 week of this high-carb experiment
- My Tresiba (basal) dose was down to 9 units.
- My insulin-to-carb ratio using Humalog was clearly 1:25 during the day and possibly as high as 1:30 in the evening. (I would’ve needed more time to experiment and confirm the exact gram ratio but it was clearly much, much higher.)
- My correction factor was the same at 1:100 but as mentioned earlier, it did seem like my corrections took effect much faster now.
- My weight loss was still at the 1-pound loss mark mentioned earlier. (Which, considering it’s only been 7 days, seems pretty reasonable and what Cyrus advocates in his program for weight-loss pace.)
Despite my declining insulin needs, I was noticing that I felt like my blood sugar was high even when it wasn’t. I felt that sort of lethargic, thirsty feeling that comes with blood sugars around 250 mg/dL or higher.
I was checking my blood sugar more often to see if I was indeed high, but I wasn’t. Even at 90 mg/dL, I just felt that icky high blood sugar feeling. And brain fog like whoa.
I also had developed a headache that wouldn’t budge with more water or Aspirin. Can I say that this headache was absolutely the result of this high-carb diet? No, but headaches are a truly rare thing for me, and this was the only change in my life at this time.
And, my digestive tract was continuing to fight off all the legumes. Gassy to the max. And while I was (TMI alert) pooping twice a day in my previous low-carb diet, I was now only pooping once a day and it was not an effortless poo, I’ll just put it that way.
But I continued to follow the program, eating entirely vegan all day long, whole foods.
Your goal on their program is to eat fewer than 30 grams of fat per day. And that might sound easy at first, but simply eating an entirely vegan diet up until dinnertime could add up to 17 grams of fat (yup, even oat bran has 4 grams of fat).
The idea of striving to meet their ultimate goal of only 20 grams of fat seemed pretty impossible, and I am amazed that women following this program can do that while still getting enough fat to maintain proper hormone levels and menstruation.
Then I ate cheese for dinner!
What I wasn’t aware of when I headed into this experiment is that the program expects your 20 to 30 grams of fat to be made up of entirely vegan foods. Using the remaining 15 grams of fat in my total allotment on Day 6 in the form of cheese for tacos in which steamed purple cabbage was my substitute for ground beef was actually not okay.
The entire rest of my day was vegan but the presence of 10 grams of fat from cheddar cheese (which put my fat quantity at 31 grams) was not allowed because it’s not “plant-based.”
(Neither were the corn tortillas because they are processed. It didn’t matter that the rest of my day was whole foods I cooked myself…the expectation was zero processed foods.)
My understanding was that as long as my fat intake was 30 grams or below (yes, I went 1 gram over), it was up to me how that dietary fat allotment was spent. But their definition of “plant-based” actually meant vegan.
Cyrus later explained that they don’t use the term “vegan” when describing or teaching their program because of the negative connotations that can go along with it. Honestly, had I known he expected 100 percent veganism, I wouldn’t have signed up for it because I firmly disagree with it — but I’m not going to start a debate on that here — it’s unnecessary and my thoughts on it aren’t unique.
Not knowing veganism was the expectation, I posted a picture proudly of my corn tacos with water-sautéed purple cabbage, cheddar cheese, and taco seasoning. I posted this picture in the Members Only “Mastering Diabetes” Facebook group.
Many of the reactions were positive and supportive–congratulating me for skipping the beef and embracing the vegetables. And sharing their personal approaches that they used to eat cheese, but over the course of weeks or months, they gave it up and don’t miss it. Along with meat, too.
(I would love to quote some of the incredibly kind and supportive comments from other members but I left the group and therefore don’t have access to those direct quotes anymore.)
And some of the reactions–primarily from coaches of the program (there are additional coaches besides Robbie and Cyrus)–came in the form of lectures that cheese is absolutely not part of this program. As well as several directions to “The goal is 20 to 30 grams of plant-based fat. Go back and review the course materials to learn how to construct a perfect dinner.”
This language and expectation of 100 percent compliance within the first week of the program left me feeling incredibly alienated and criticized. I knew that even while continuing with the program, I wouldn’t be posting any more pictures or trying to engage in discussion about my personal experience.
I want to note that this same kind of unfriendly interaction could easily happen in a ketogenic group if someone said they ate fruit. It’s a “100% or nothing” kind of mentality that simply doesn’t work well for me, but it does work well for some others.
Anyway: I went to bed that night with a blood sugar of 60 mg/dL, which I treated with 8 grams of carbs and went to bed.
I woke up in the morning with a blood sugar of 350 mg/dL–which was clearly a direct result of the cheddar cheese. When I told Cyrus about this spike, he assured me that it was incredibly normal and what he would expect to see when you eat 10 grams of fat from saturated fat rather than plant-based fats. The fat, simply put, causes a tremendous spike in my blood sugar over the course of hours.
Do I want to be on a diet that makes my body overreact so severely to saturated fat that one serving of cheese suddenly spikes my blood sugar by 200 points?
This is another area where I really disagree with Cyrus’ and Robbie’s approach in that they’ve concluded that this means people with diabetes shouldn’t eat saturated fats or even most sources of fat because clearly, they raise blood sugar.
But I can tell you that in my normal low-carb eating approach, I could easily eat 10 grams of cheddar cheese and my blood sugar would not rise at all. Instead, the carbs would be what caused a dramatic spike in blood sugar.
- The extreme route with the ketogenic diet is to wipe out all carbs because “they raise blood sugar.”
- The extreme route within Cyrus and Robbie’s approach is to wipe out all fats because “they raise blood sugar.”
In reality, it seems to me that the extreme reaction from one macronutrient is a direct result of the extreme consumption of another macronutrient.
I could easily argue that Cyrus and Robbie’s approach to eating so many carbs makes me way too reactive to fats, which raises my blood sugar and thus means I shouldn’t eat so many carbs.
By Day 9: I felt like one big starchy bean. My blood sugar felt high all day even though it wasn’t. I felt foggy and thirsty. And I was confident in what was causing this: this high-carb diet. I felt like my veins were full of starch. And that headache that started on Day 7 was still rocking hard.
And that’s when I decided that starting on Day 10, I would transition back to a lower-carb eating with a newfound understanding of/or appreciation for:
- Using my new air-fryer! (I have been cooking nearly everything in this and I love it! )
- Feeling incredibly grateful for the clarity and constant energy that comes with a disciplined lower-carb diet
- Make an extra effort to ensure that my low-carb eating consists of lots of vegetables
- Cyrus talked to me in great detail about the immense value of making sure you are rotating your insulin injection (or pump) sites. The more you inject into one area, the more scar tissue and thus insulin resistance will result. I’m pretty lazy about rotating, so this is a valuable lesson and reminder that I will strive to carry forward.
- Feeling re-motivated to reduce the treats I was eating in March and lose that final 10 pounds that’s clinging mostly to where those two babies of mine were pulled from via c-section. Losing those 10 lbs would get me to a leanness that would enable me to see my abs and that’s simply a fun goal.
By Day 10: I fasted until 1 p.m. and then ate a meal of 2 eggs over-hard with a giant bowl of veggies from my air-fryer (which I would normally have just steamed and lightly oiled in a pan). I didn’t feel hungry again for hours after that meal. By the time 4 p.m. came around, that thick starchy feeling was subsiding and I was starting to find my natural energy and clarity from a lower-carb approach to eating.
I realize that I definitely did not give this approach of eating as much time as Cyrus would have preferred before I came to any conclusions, but I honestly felt so lethargic and “starchy” that I couldn’t keep doing it. It’s not the right fit for me. And YES, it absolutely did make me more sensitive to insulin but the trade-off, for me, wasn’t worth it.
UPDATE: By Day 20: Transitioning back to my usual eating took a little “eating anything” route for a few days (maybe days 11 through 14) where I just truly felt like my body wanted to eat anything that was gluten-free and calorie-dense, perhaps to compensate for the ultra low-fat intake of 10 days.
A rebound, for sure. But, I also started exercising again–only then did I realize that during my high-carb, low-fat experiment my energy felt a bit more precarious and I hadn’t had the energy stores to feel like jumping rope regularly. I could feel my body so thoroughly burning through everything I ate, the idea of exercising was just passively unappealing.
By Day 15 of eating “my” way, I was jumping rope again every day, for up to 45 minutes and feeling very energetic. (I recently realized I can do this form of exercise in my living room, while the baby is napping and the toddler is playing, while fasted, and it doesn’t cause any issues with my fibromyalgia sensitivities!)
Insulin Doses, Weight-Loss, etc.
- I’ve also lost another pound, down to 123. Eating between 1600 to 2000 calories based on how much jump-roping I did and overall hunger cues!
- I raised my Tresiba background insulin dose to 10 units initially, but I’m back down to 9 units. I’m considering dropping to 8 units as I type this because I’ve had recurring lows over the past 24 hours.
- My carb ratio is about 1:15 or 1:20 depending on when I last jumped rope!
- My correction factor is out-of-control sensitive which is why it’s definitely time to first adjust my basal insulin dose (mentioned above) and then see where my correction factor is. A correction factor of 1:150+ is a big, big sign that there’s too much basal on board.
- I’ve been eating my whole-foods, fairly high-fat diet. Carb intake is about 100 net carbs, but I’ve had a few days that were higher, too, around 150 net carbs.
- Real food. Plenty of fats. Lots of veggies. Some meat. Some fruit. Avoiding sugar or “treats” except for the weekend and those are treats I baked myself. Or my favorite gluten-free pizza! PIZZA! AHHH! I love pizza.
- ..TMI…my bowel movements are back to their usual, effortless, happy selves. (Yes, I just gave bowel movements their own identity and emotion.)
By Day 25: Eating delicious things like homemade pumpkin chocolate mousse (with real sugar), my background insulin dose is now down to 7 units…because of jumping rope for 30 to 45 minutes a day! Holy insulin sensitivity, Batman! Why bother with an extremely restrictive diet when jumping rope makes insulin like super juice? Loving it.
In a sense, it comes down to which argument you like best because we can find a zillion studies that support each side’s argument: eat less fat and more carbs vs. eat more fat and less carbs.
Cyrus and Robbie argue that ketogenic and low-carb diets that consist of large quantities of fat lead to heart disease, high triglycerides, and high cholesterol but there are plenty of cases of research proving this to be an outdated myth and misconception.
Pro-Fat Arguments, Studies & Experts
Here are just a few of those studies and arguments from experts why fat does not raise your risk of heart disease and cholesterol…
A great place to start reading is how the philosophy of low-fat philosophies actually began in this document from the History of Medicine & Allied Sciences.
- The Diet-Heart Myth: Cholesterol and Saturated Fat Are Not the …
- Cholesterol | The Nutrition Source | Harvard T.H. Chan School of …
- Rethinking dietary cholesterol. – NCBI
- Why Eggs Don’t Cause Heart Attacks – DiabetesDaily
- Everyone Was Wrong: Saturated Fat Can Be Good for You | Greatist
- Large diet study suggests it’s carbs, not fats, that are bad for your …
There are tons and tons of people who are thriving on low-carb or ketogenic diets. Their lab work easily disproves the myth that “dietary fat raises cholesterol levels.”
We could go on and on arguing about this but the fact is that people have now been eating this way for years and many are reporting great results and great health.
Pro-Carb Arguments, Studies, and Experts
And then, there are a variety of arguments trying to make the case for a low-fat diet, too…and with that are tons of people who feel best on this type of eating rather than low-carb eating!
- The China Study – T. Colin Campbell Center for Nutrition Studies
- Q & A with Dr. Neal Barnard – Vegetarian Times
- The Evidence for Saturated Fat and for Sugar Related to Coronary Heart Disease
- Interview with Cyrus Khambatta on Treating Diabetes with High-Carb/Low-Fat
- Doug Graham’s Raw Food Philosophy
- (I honestly had trouble finding more studies because every time I googled “low-fat diets and high cholesterol,” I just got more results for why dietary fat does not lead to high cholesterol.)
So, Can’t We All Just Get Along?
Does there have to be only one way to eat for health? Must we promote our own approach only by bashing someone else’s?
I do wish that Cyrus and Robbie would consider offering a more middle-ground approach for people who want to learn how to better incorporate carbs in their diet without becoming severely low-fat vegan. And that their online community, in general, would be open to “less than perfect” meals so that those who aren’t on board with being fully vegan could still be part of that higher-carb community and supportive discussion.
I also wish that both sides could appreciate the simple fact that there is more than one way to be healthy in life with diabetes. Your plan does not succeed based on the failure of another plan. We all respond differently to different approaches…and that’s really okay.
I’ve been directing people to Cyrus’ site for years whenever I hear come across someone expressing frustration that low-carb isn’t working for them or that they simply don’t want to eat that way. I wish the two extremes of eating could respect each other’s differences and appreciate each other’s passionate devotion to what works best for them.
I tip my hat to all the high-carbers and all the low-carbers, because both require tremendous discipline.
Personally, I’m finding the extreme swing in either direction to be the biggest turn-off for me at this time in my life, and in my own health, it feels unnecessary. There is a middle ground. It’s very possible to eat a lot of plant-based foods on a lower-carb diet. Which personally feels far more balanced to me. And why on earth must I completely give up gluten-free pizza just to obtain ultra-sensitivity to insulin when I wasn’t struggling with insulin resistance in the first place?
FACT: Carbs do raise blood sugar. But it’s very easy to survive without them because your body will convert more protein into glucose for additional fuel, and burn ketones for fuel if carb intake is low enough. Burning ketones for fuel has proven to be very safe and effective, even treating conditions like epilepsy. Babies are in and out of ketosis regularly, even when breastfeeding.
- At the same time: there are many people for whom a low-carb or ketogenic diet simply doesn’t work for any variety of reasons. They thrive eating this high-carb, plant-based, low-fat approach. And that’s great!
FACT: Fats do cause varying degrees of insulin resistance. But does that mean fats are the enemy? The body cannot function without fats. This is a fact.
- And there are many people for whom eating a vegan diet led to a variety of extremely negative symptoms. Eating a low-carb, higher-fat diet leads to awesome energy, better blood sugars, and sustainable weight loss. And that’s great, too!
Fortunately, you get to choose how you eat. You get to experiment and see what feels right to you. Why must everyone follow the same protocol?
Achieving ultra-sensitivity to insulin does not automatically equal health in the same way that achieving flat-lined blood sugars through a ketogenic diet doesn’t automatically equal health. Your health is more complex than that.
I’m happy I was open to experimenting, but what I’d love to see next is how my pal Cyrus felt on a low-carb diet! Although, I think asking him to try that might be asking too much.
Regardless, I admire Cyrus and Robbie’s passionate dedication to their own philosophies on food and thriving with diabetes. They’re clearly helping many people with their program–and that’s what matters! Find what works for you, be open to experimenting, and never stop learning and studying your own diabetes.
If you are interested in eating a high-carb, low-fat vegan diet, I highly recommend checking them out at MasteringDiabetes.org. They are passionate, genuine, and eager to teach more people their unique approach to eating.
Personally, I think a large majority of people don’t do well with the extremes of ketogenic or this low-fat vegan approach. Both eliminate tons of different types of food, are hard to sustain long-term, make social food-related gatherings feel awkward and impossible, and heck, they take a lot of the FUN out of so many delicious foods the world has to offer!
I think a large majority of us, diabetic or not, would thrive from focusing on a few simple things:
- More veggies
- More whole foods
- Fewer processed products
- Less alcohol
- Fewer $7 coffees from Starbucks that contain 80 grams of sugar
- Just more real food in thoughtful moderation with a twist in quantity that you know works well for you.
- And room for the occasional treat like ice cream, pizza, or tacos! If that’s what works for you!
What works best for YOU? Listen to your body and create your own success.





Pam Olsen
I am a new type 2 diabetic whose doctor is INSISTING that I follow the Mastering Diabetes way. I don’t think this is for me. I feel that humans require a certain amount of animal protein. I also feel she is running me around the mulberry bush for her own beliefs. I will be searching for a new, more middle of the road provider. Thanks for your article, it has provided me with more confidence to get on my own diabetes journey, my way.