This post may contain affiliate links. Please read our disclosure.
Did you know that your carb sensitivity changes throughout the day? It does, and this can have a big impact on your diabetes management.

If you are an insulin-dependent diabetic like me, you probably have some sort of system through which you estimate how many units of insulin you need to bolus for a meal.
Perhaps you count carbs, dose based on total calories, use a sliding scale, or simply estimate how much insulin you need based on your experience.
However, I often find that people are missing a very important piece of the puzzle, which is that your calculation should take into account how sensitive you are to carbs during the day.
As Gary Scheiner describes in his book Think Like A Pancreas (I posted the relevant excerpt in the post Managing Dawn Phenomenon with Basal Insulin), our basal insulin needs will vary throughout the day and I’ve found my sensitivity to carbs to vary tremendously as well.
How do I know this? Well, because I’ll need more insulin to cover a given amount of carbs in the morning than I do for the exact same type and amount of carbs at night.
Why it is important to know your different carb sensitivities
First and foremost, getting your different sensitivities nailed down is super important if you want to manage your diabetes as tightly as possible. If you don’t know what’s going on throughout the day, you’ll end up over and/or under-dosing a lot.
From a general health and fitness perspective, this if far from optimal, and has the risk of putting you on a roller coaster of low and high blood sugar all day long. Not only is this very tiring, but it can also be extremely frustrating not understanding why you are running high or low all the time.
Let’s say that you work out in the afternoon and you calculate your pre-workout dose using the same formula that you use in the morning. If you are like me, and have a higher insulin need in the morning, you would most likely end up over-dosing. And we all know what that means. You have to skip the workout or eat extra carbs that you had not planned for or want.
How to find your different carb sensitivities and keep track of them
Remember how we used my Blood Glucose Tracker to learn how to reduce the risk of low blood sugars during cardio workouts in my post about food and insulin around workouts? The same principles apply to finding your different carb sensitivities.
I suggest keeping track for of your blood sugars for about a week, and trying to keep everything as constant as possible (food, exercise, sleep, daily routine, etc.). Then, test to find your carb sensitivity at different times during the day.
The way to do this is by measuring your blood sugar before you eat and writing it down, along with what you ate. Then measure again 90 minutes later. If your blood sugar is consistently within range 90 minutes after your meal, your dose is on point. If not, then you need to make changes.
These changes can be made in collaboration with your medical team, but you need to bring them the data. If you don’t, they won’t know what changes to make.
I’m self-managed, meaning that I make changes to my diabetes management on my own, and daily if needed. I check in with my endo regularly, but being self-managed has improved my quality of life and diabetes management tremendously, especially given how much my workouts affect my insulin needs.
How to track and adjust for carb sensitivities
If you use an insulin pump, go into your settings, and you’ll see that your pump actually allows for up to 6 different carb and correction factor settings. You may not be using them today, but there is a reason why pump manufacturers put that option in there.
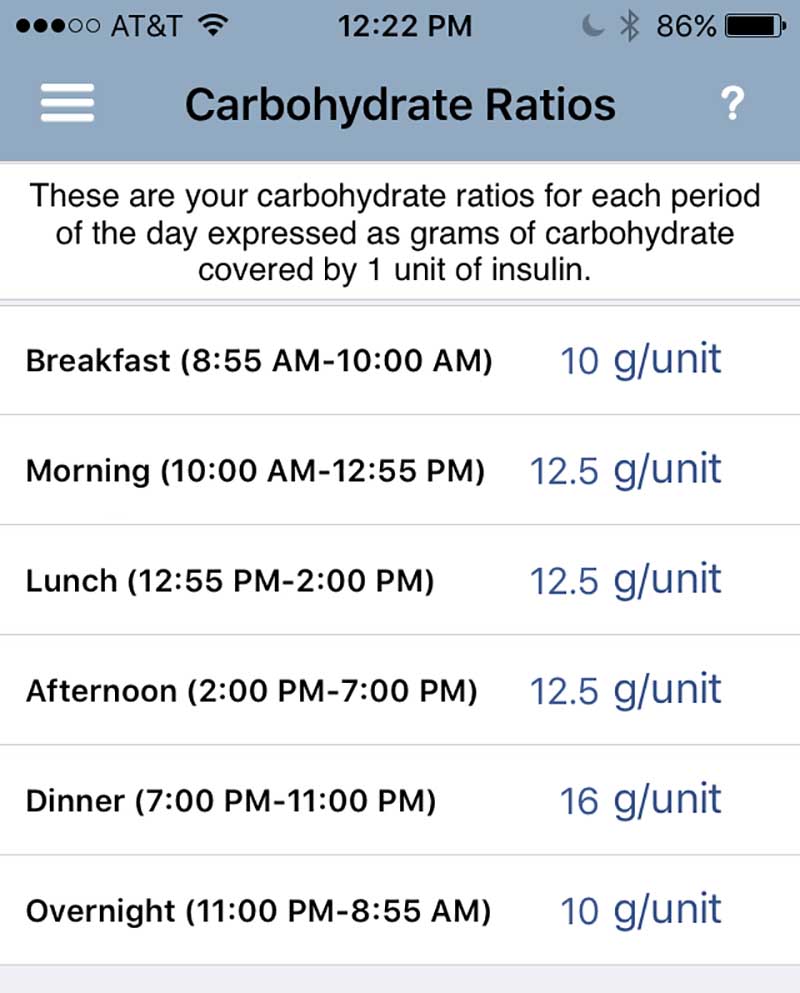
If you are on pen therapy, like I am, you either have to keep track of it all in your head (LOL! That would require more brain capacity than I have) or use some sort of calculator. In the past, I’ve used the RapidCalc app to keep track of it all. What you see below is a screenshot of my current settings.
It’s set up pretty much like a pump, so you just enter all your information and it will calculate your recommended dose based on time of day and active insulin, just like a pump.
As you can see, I’m not utilizing all 6 settings right now, and only have 3 different ratios, with my 11 PM – 10 AM period requiring the most insulin.
The 10 g/unit means that I’ll need 1 unit of insulin per 10 g of carbs during that period, while I’ll only need 1 unit of insulin for 16 g of carbs in the evening.
If you already have the basic blood sugar management under control, I suggest you sharpen your diabetes management skills by finding you different daily ratios. Knowing what’s going on just makes life easier, and you’ll ultimately be spending less time correcting and worrying about low or high blood sugar.
Suggested next post: No Carb, Low Carb, or Moderate Carb – Which is the Best Diabetic Diet?




Peter Keep
Good article – unfortunately the Google play store says about GlucoLog RapidCalc : “this app isn’t avaiable in your region”. (State of Washington?)
Oh well. Still a good article.
Christel Oerum, MS
Yes, RapidCalc was unfortunately taken off the U.S apple store. You can still download it though (and for free), if you download it from an EU app store. Here’s how you do that: https://thevpn.guru/install-apps-different-country-ios/
Once downloaded you can change your settings back to U.S
Marlene Nicholson
My insulin sensitivity differs depending on whether by BG is high, low, or normal. E.g. assume my bg is 200 before dosing before a meal. If I dose for the carbs in the meal plus a correction to reduce by bg to the normal range e.g. 120 the dose is insufficient and my bg will stay high for hours. It is as if my bg gets “stuck” if it is in the high range. A similar thing happens if I am low. The only way I can deal with this is to add more insulin (and it is hard to know how much more. So I rarely eat when my BG is high–I wait until the dose brings it in the normal range–which is a pain if you are eating with others, and/or are very hungry. I never see other type ones mention this. One of my doctors said it was quite common–don’t know if he was just humoring me. (Of course I always take into consideration my active insulin when calculating my dose)
Christel Oerum
I know what you mean. I call them stubborn highs as they can seem really hard to get down without a lot of additional insulin. I haven’t seen it described in any medical literature though (but can’t say I’ve looked either)
Kim
Interested bystander here, wondering if the stubborn highs can be due to a. High carbs in the previous meals saturating all glycogen stores, or b. Cold skin and extremity temperature which reduces peripheral and superficial tissue sensitivity to insulin?
Christel Oerum
In my experience how many carbs are stored in muscles and liver has a big impact on how much insulin is needed to cover meals and corrections. Generally, if I go through periods where I eat more carb-heavy I’ll overall need more insulin, not just for meals.
Temperature has also shown to impact insulin sensitivity, so I think your observations are valid
Tina Derke
Oh, my God! This is my problem more often than not. Sometimes it seems as if the insulin is just not received. I didn’t know it was “quite common” and am always anxious about it.
Rohana
I’m a 75 yr old kidney transplant patient who became diabetic immediately after my transplant. This type of diabetes (“NODAT”) can mimic characteristics of type 1. For me, I can wake with 100, drink coffee no sugar, 1 wasa and 1 oz cheese, jump to 220, still needing more nutrition! It’s like trying to stay on a bucking horse! I am so grateful to be using a Dexcom meter oh, no need for a pump in my case. I use SparkPeople 2 record and get data on every item of food I eat. It’s the best I’ve tried. If not for the Dexcom I would have continued to have very frightening irregular glucose levels. I used to have dangerous rapid drops in my glucose level . Thank goodness I haven’t had to call 911 and the meter allows me to teach myself my response patterns throughout the day. I wish that endocrinologists would pay more attention to coaching people with post-transplant caused diabetes. I had to learn all this myself over these years thanks to diabetics doing a fantastic job on YouTube. Now, I am appreciative of the excellent informative articles you are posting!!!
I have a couple of favorites who are experienced patients, in professional health care and training. Extraordinary supportive and educational individuals, it’s free, great help! BTW, I have been referred to as “most proactive patient”, miracle survivor, etc. Since I got and beat cancer, against the odds, 40 yrs ago and working hard to live with the resulting co-morbidities. I wish others were as motivated to help themselves control this awful disease.
Christel Oerum
You sound amazing! What a story. Thank you for sharing, being proactive with your health is probably why you’re doing so well today
Adam Garnesh
It’s really important to maintain your curb in your diet effectively to avoid extra fat and calories. Very nice blog. Well-described Content.
shiza khan
wow nice information, i am from pakistan and in pakistan people didn’t care about diabetes keep updating the information thanks you
Shaun
Hi Christel,
So how are you determining your carb ratios for “each time of the day” though? Ive always been taught the standard 1800/TDD=ISF, and 500/TDD=I:C. But like you said, that does not work for every time of the day, as that is an average of the whole day instead… the only indicator I know of each time in order to make a dosing change is to acknowledge if Ive over-dosed or under-dosed an hour after the meal… this still does not help me fine tune the math without more “guess work” since I am going to have to either remove or add a unit or two each time in order to see if that adjustment works… but then I still dont know my new ratio on paper. Is there a specific formula you are using to obtain each part of the days new ratios? That would be a big help.
Christel Oerum
I’ll usually stick with the same meal for a few days when I think I need an adjustment. FOr example, I’ll eat the same thing for breakfast for a few days, take detailed notes and adjust accordingly. You of course also have to take any corrections + high or low blood sugars into account. Sometimes it happens more organically where I’ll notice that I start running high or low ~2 hours after a meal and I know I need an adjustment to my ratio
Shaun
ahhh ok, this is what I do already as well… Im a dumb dumb though, and want a way to make sense of it mathematically, rather than just recognizing I need to move my I:C or ISF numbers up or down by guess in my calculator app based on my observations. I thought maybe there was a mathmatical way to do it in the short term, vs an average of the whole day. Thanks Christel.
shelly
I am so excited I found your site. I am also a type 1 diabetic and have been now for 48 years and I love to watch what I eat and work out, But lately I am starting to run into some complications with balancing my food, my work outs, and my blood sugar. I am on a Dexcom and love it. I have been on an insulin pump now for the last 6 years amd am noticing I am putting on weight and fat where I am wearing my pump. I do not like it atall and searching for answers and wondering if you no anyone else noticing this? same issue? and why do you not wear an insulin pump? for this reason?
Christel Oerum
Hi Shelly – so glad you enjoy the site!
I haven’t seen any research on injections causing more fat accumulation in certain areas but know of many who feel like they have more fat in the areas where they inject/pump. Maybe more aggressive site rotation could help you.
Me not wearing a pump is 100% related to preference/life style. I understand the benefits of a pump and why most people love it, but I have good control with pens and this regime works for me at this time in my life.
Diane Barrieau
Hi, I’m confused. You said “with my 11 PM – 10 AM period requiring the most insulin. The 10 g/unit means that I’ll need 1 unit of insulin per 10 g of carbs during that period, while I’ll only need 1 unit of insulin for 16 g of carbs in the evening”, but the graph looks like your greatest use is during the evening, requiring 1 unit/16 g of carbs vs. 1 unit/10g carbs from 11pm – 10am. Am I reading this wrong? Thanks for clarifying!
Christel Oerum
The picture of my settings shows when I use different ratios. The timeslots from 1) 8:55 AM-10:00 AM and 2) 11 PM -8:55 AM, shows that I for this time range need one unit to cover 10 g of carbohydrates. At all other times, 1 unit of insulin will cover 12.5-16 grams of carbohydrates. So think of it like this from 11 Pm- 10 AM I can eat a meal of 30-grams carbohydrates and will need 3 units to cover that. If I’d eaten that amount at other times of day I would have needed 2.4- 1.9 units only. The higher the ratio the less insulin. I know it can be a little hard turning that one around in your head. So the way to calculate it is to take the amount of carbs and divide it by your ratio, then you know how many units you’ll need