This post may contain affiliate links. Please read our disclosure.
Being a pharmacist, I have often been asked if it’s safe to use expired insulin and how to tell if insulin has gone bad from exposure to heat or cold.
Medications have an expiration date because their stability cannot be guaranteed, based on clinical studies, past that date.
Taking a chance on eating an expired food product is one thing; it’s quite another taking a chance on insulin that may not work at maximum capacity, and therefore may cause harm to your overall health.
Can you still use insulin after the expiration date?
Using expired insulin is absolutely not recommended and should only be done if you have no other option.
The effectiveness of insulin degrades over time and it’s impossible to predict how well expired insulin will work – or if it will even work at all!
Insulin is a bit unusual in that it had two expiration dates; one is the expiration date if insulin is unopened and stored at the proper temperature. The second expiration date is the date the manufacturer suggests insulin is good for after opening and when kept at room temperature.
Be sure to check both dates so you know if your insulin is still safe to use.
What happens if you use expired insulin?
When insulin is not working properly, it’s akin to what happens upon an initial diabetes diagnosis when your pancreas is not producing adequate insulin for your body’s needs.
Blood sugars start to rise and can do so quite rapidly. When you see blood sugars go up and have ruled out other causes, such as illness, changes in diet and/or exercise, or new medications, start to suspect that your insulin has gone bad.
When you switch to a new vial or pen and your blood sugars “magically” go back to normal, you have verified that your insulin was in fact damaged.
It’s important to note that insulin can go bad before its expiration date. This happens very rarely, but if you feel that your insulin isn’t working as well as it should, try switching to a new vial or pen.
How can you tell if insulin has gone bad?
There are two ways in which you can tell if your insulin has gone bad.
The first method is visual inspection. If your insulin looks cloudy or discolored in any way, don’t use it. If it has clumps or what look like little “strings” in it, it’s probably not safe to use.
The second way to know your insulin is not working properly is unexplained high blood sugars, as mentioned above.
How to store insulin
Proper insulin storage is important to ensure that the insulin stays effective.
Avoid exposing insulin products to extreme temperatures. Insulin is a protein and this makes it subject to degradation (breakdown) when temperatures are too hot or too cold. Additionally, keep insulin products away from direct sunlight as this can also cause a breakdown of the insulin.
Proper insulin storage is so important that the FDA recently took action to ensure that Insulin pens must always be dispensed in their “original boxes” so that instructions for the proper use and storage of insulin are always included. This means that your pharmacy is not allowed to give you just 2 insulin pens from a box of 6 pens.
Insulin that is not being used should be stored in the refrigerator at 36°F to 46°F (2°C to 8°C), a safe distance away from the back and top of the refrigerator where cooling elements may cause the temperature to approach freezing.
The refrigerator’s butter compartment or produce drawer is typically a good option for insulin storage.
Update: A new study from 2021 shows that insulin stored at 77° to 98.6°F (25°C to 37°C) for four weeks showed the same stability as insulin stored at the currently recommended pharmaceutical protocols of 36° to 46°F (2°C to 8°C) until opened.
Any insulin vials or pen that are “in use” can be stored outside of the refrigerator at temperatures up to 86F or 30C (always check manufacturer product inserts for exact instructions).
The reason for storing in-use insulin at room temperature is that cold insulin can produce a more painful injection.
When should you throw away an open insulin vial or pen?
Many insulin pens can last outside of the refrigerator for 7-28 days, in some cases even more.
Here are some specific recommendations for insulin storage that you can follow. As always, check the instructions inside the box for specific guidance.
New insulins are coming to market at a rapid pace, and the instructions may vary slightly with different formulations and brands.
All times below are from when you open the vial or pen.
- Insulin Glargine (Basaglar®): Throw away pen/vials after 28 days.
- Insulin Lispro (Humalog®): Throw away pen/vials after 28 days of use.
- Humulin R: Throw away vials after 31 days of use. If pen, throw away after 28 days.
- Humulin N: Throw away vials after 31 days of use. If pen, throw away after 14 days.
- Humulin 70/30: Throw away vials after 31 days of use. If pen, throw away after 10 days, even if it still has insulin left in it.
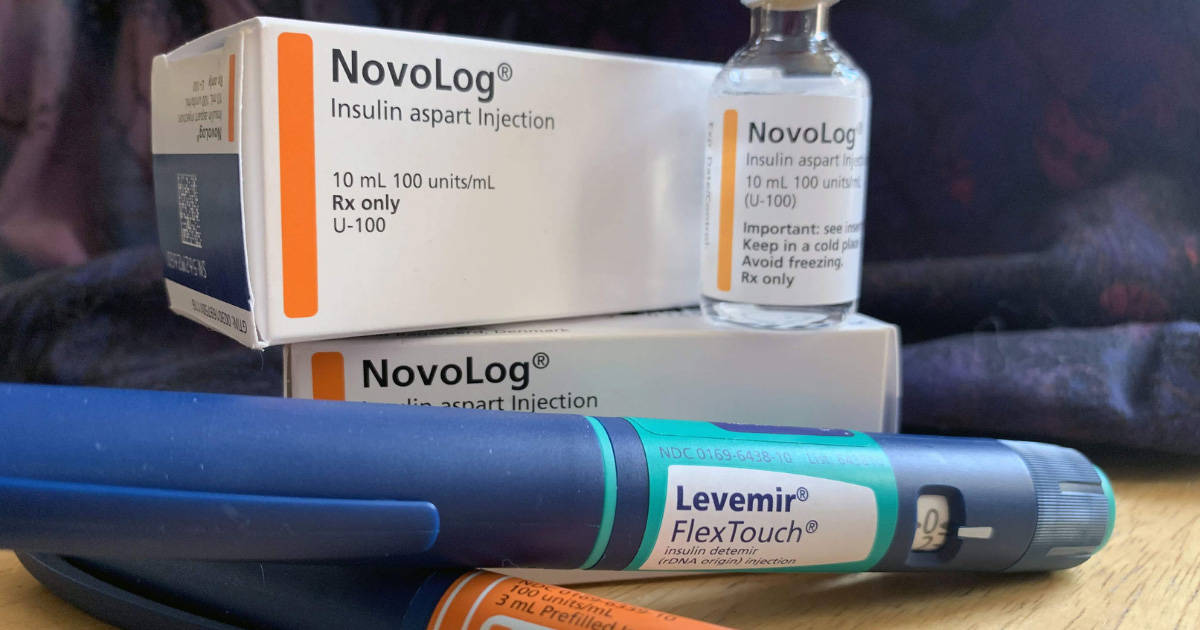
- Insulin aspart (Fiasp®, Novolog®, NovoRapid®): Pen and vial, throw away after 28 days.
- Insulin degludec injection (Tresiba®): Pen and vial, throw away after 56 days.
- Insulin detemir injection (Levemir®): Pen and vial, throw away after 42 days.
- Isophane insulin human suspension (Novilin® N NPH): Vial – 42 days; pen – 28 days.
- Insulin human injection (Novolin® R): Vial – 42 days; pen – 28 days.
- 70% human insulin isophane suspension and 30% human insulin injection (Novolin® 70/30): Vial – 42 days; pen – 28 days.
- Novolin NPH and R also represent the ReliOn ® brand available at Wal-Mart.
- Insulin lispro injection (Admelog®): Pen and vial, throw away after 28 days
- Insulin glulisine injection (Apidra®): 28 days
- Insulin glargine injection (Lantus®): 28 days
- Insulin glargine injection (Toujeo®): 28 days
For questions about a particular brand of insulin, problems, or concerns about product stability, contact the manufacturer for help (links above), and in some cases, ask for a replacement.
Products to help store insulin safely
Just as new insulins have rapidly been developed, more efficient methods of keeping insulin safe have evolved as well.
Three such products have now come forward with unique and simple ways to carry insulin products with you, whether it be on short hikes, or traveling the world.
MedAngel is a handy “smart thermometer” for medications that need to be stored at certain temperature ranges. You keep it next to your insulin and it will alert you on your phone if the temperature is out of range. You can customize the temperature range for your specific medication, which is great.
Frio Cooling Packs can work up to 5 times longer than ice packs and seem to keep insulin products at a more consistent temperature. They can last up to 45 hours or more and are easy to store and use, coming in a variety of styles and colors. They require soaking in water before use as instructed on the website.
The Vivi Cap is a cooling device for insulin pens. It simply clicks onto an insulin pen instead of the cap and with the push of a button, the device then works to keep insulin at the proper temperature for as long as you need it to. No ice packs or preparation is necessary. The battery lasts as long as the device, which can be active for several years.



PATRICIA rodman
my pens are dated march 21 2025. Can I still use and for how long
Christel Oerum, MS
Insulin that’s too old might not lower blood sugars as expected. You could ask your doctor. If it were me, I’d continue to use it and stop if it didn’t seem to work as it should.
Can Fireworks Expire
This is a really cool page. One of the best posts I’ve come across in quite a while. I hope to see more content like this.
Leonard Morris
How long can unopened Humalog last in the Refrigerator? Where should it be kept in the Refrigerator?
Christel Oerum, MS
You’ll find the expiration date on the pen/vial/box. It can be kept anywhere in the refrigerator but if you have an older fridge I wouldn’t leave it directly up against the cooling back/cooling element
Bill Vosburgh
This and similar articles miss the point that bio-lab created insulin goes bad unpredictably but frequently at much shorter periods than the claimed 28 or so days.
I keep records of when NovoLog or Tresiba pens go bad, Lot #, Exp. Date and how many days (or hours) since I started using the pens. My records go back to 2017 when I started using vials but quickly learned the insulin loses potency so quickly I was wasting my insurer’s money and switched to pens.
I use syringes with pens because 1/4″ pen needles are so short they cause ‘tunneling’ (insulin leaks out the injection path).
Times for pens going bad range from a high of 24 days down to two or three days. I keep pens refrigerated from when I get them and while in use.
Unstable insulin is a result of altering the natural human insulin amino acid structure to get patents and 20 years of monopoly price protection.
FDA also approved Thalidomide, AZT and COVID injections. It’s call allopathic medicine for good reason.
MT Hannigan
The article states that throwing Lily insulin away after XX days of “use”, which I take to mean after you have opened the pen, vial, etc. But for Novo Nordisk insulin, “after use” is not specified. Can you be more specific about whether it is after opening the insulin?
I have always assumed that unopened insulin is okay to use until the expiration date, as long as it is stored in the refrigerator.
Tobias Oerum
Thank you for the feedback. We have updated the text to make it clearer that all times are from you open the vial or pen.
Vivian Parramore
You say that there are two expiation dates on insulin. The date on the box is the same as the date on the pen. If I am understanding correctly, please tell me where I can find the second expiration date.
Christel Oerum
What is meant that the expiration date printed on the pen and the box are for unopened insulin that’s stored in the refrigerator. An opened insulin pen is usually only good for 28 days (check the manufacturer label) so the second expiration date will be (most likely) 28 days after the pen/cartridge/vial has been opened.
Meaux
I have some 3 year old Lantus, never been opened, stored in fridge to use for backup. I have 1 that has been half used and it is still crystal clear… Should I ditch it or keep it stored??
Christel Oerum
I don’t think I would. It might not hurt you but it might not work as it should. So if you do decide to try it, you’ll have to keep a close eye on whether it’s actually lowering your blood sugar
DeMarcia Hamilton
I accidently left my insulin pen in the car on a hot day, 90 degress. Pen was 10% used.
Is it stilll good
Christel Oerum
Potentially it won’t be effective in lowering your blood sugars anymore. It’s your choice but I would discard it and start a new pen
Tomi
Hello I would like to know do the same rules apply for trulicity pins that have an expiration date of November 2023?
They have been in the refrigerator unopened in the boxes the whole time…
Christel Oerum
Yes, generally you don’t want to use expired insulin
Jim
I’ve used out dated fast acting Novolog for many years and mostly kept it in the fridge but some in the freezer and so far it has always done the job for me.
Some for as long as 10 years. All have worked well.
Dorothy
I have insulin in my refrigerator for my ex, who sometimes stays with me. His assisted living facility controls the rest of it. So, is it okay for me to use it, and then put it back in the refrigerator when he goes away, and keep it for more than 28 days? The truth is, I have been doing this, but I now have a pen of soliqua that technically expired last month
Christel Oerum
You’re supposed to only use an open pen/vial for 28 days and then change it out as the efficiency degrades over time. It shouldn’t matter a whole lot if it goes in and out of the fridge. That being said, it might still work, but it can not be guaranteed which can make it a dangerous solution
Adam
You can but it’s really tough to say whether it’s going to be effective or not. There’s no hard and fast rule. I’ve used insulin months after the date on the vial has expired and it still works.