While low blood glucose (hypoglycemia) might seem like an excuse to eat candy, for those with diabetes, it’s far from fun. Hypoglycemia can disrupt daily activities, cause dangerous situations like while driving, and leave you feeling shaky and panicked.
This article covers symptoms, causes, treatment, and prevention of low blood sugar.
Key Points:
- Low blood glucose (sugar) occurs when blood sugar levels drop below 70 mg/dL, leading to physical and mental impairment.
- Common symptoms of low blood sugar include shakiness, sweating, confusion, and dizziness.
- Hypoglycemia unawareness can develop over time, making it difficult for some people to detect low blood sugar symptoms.
- Management of lows involves using fast-acting carbohydrates, monitoring, and adjusting insulin doses as needed.
What is low blood sugar?
In people without diabetes, blood sugar levels rarely fall below 70 mg/dL.
When they do, the body begins to struggle with even basic functions. The brain, which depends on a constant supply of glucose for both physical and mental processes, can quickly become impaired.
If left untreated, low blood glucose can lead to severe complications, including seizures and even death.
Read more in: What Are Normal Blood Sugar Levels? and Blood Sugar Chart: Blood Sugar and A1c Targets.
What are the signs and symptoms of low blood sugar?
There are several key signs that your blood glucose has dropped below a safe level. According to the American Diabetes Association (ADA), symptoms of lows include:
- Feeling shaky
- Nervousness or anxiety
- Sweating, chills, and clamminess
- Irritability or impatience
- Confusion
- Fast heartbeat
- Lightheadedness or dizziness
- Hunger
- Nausea
- Pallor (color draining from the skin)
- Sleepiness
- Weakness or lack of energy
- Blurred or impaired vision
- Tingling or numbness in the lips, tongue, or cheeks
- Headaches
- Clumsiness or coordination problems
- Nightmares or crying out during sleep
- Seizures
You may also experience other unique symptoms. For instance, when my blood sugar drops during exercise, my thighs feel numb and tingly. It’s important to recognize your own early signs of hypoglycemia so you can treat it promptly.
Hypoglycemia unawareness
For some people, particularly those with long-term diabetes, “hypoglycemia unawareness” can develop. This occurs when your body no longer signals low blood sugar, increasing the risk of severe lows and seizures.
According to the ADA, it is possible to regain early warning symptoms of low blood glucose by avoiding hypoglycemia for several weeks. This may require temporarily raising your blood sugar targets, which should be discussed with your healthcare team.
To manage hypoglycemia unawareness, consider using a continuous glucose monitor (CGM), which can alert you to low blood sugar before it becomes dangerous.
Also, raising your target blood sugar slightly, such as aiming for 100-110 mg/dL instead of 90 mg/dL, can reduce the risk of severe lows.
Learn more about this condition in: Understanding Hypoglycemia Unawareness.
Symptoms of low blood sugar when you aren’t actually low…
For people with diabetes who have had consistently high blood glucose levels (A1c above 8 percent) or those dealing with diabulimia, the body can acclimate to these higher levels. When blood sugar starts to come down to a healthier range, it may trigger false symptoms of low blood sugar.
Reversing this issue takes time. If you’re dealing with diabulimia, reach out to your healthcare team for support.
Work with your certified diabetes care and education specialist (CDCES) to gradually lower your blood sugar targets, allowing your body to acclimate to healthier levels without triggering false lows.
What causes low blood sugar?
In people with type 1 and type 2 diabetes, lows usually result from an imbalance of food, activity, and insulin or other diabetes medications.
Exercise without adjusting insulin or carbs
Activities like walking after a meal can cause a severe drop in blood sugar if insulin isn’t adjusted, as the body burns glucose faster.
Inaccurate insulin dosing for carbs
Misjudging the insulin needed for meals, like dosing for a medium apple but needing less, can easily lead to low blood sugar.
Tip: Use tools like CalorieKing to double-check carb counts.
Weight loss increasing insulin sensitivity
Losing as little as 5 pounds can make your body more sensitive to insulin, leading to frequent lows.
Tip: Talk to your CDCES about basal and carb-ratio testing.
Changing insulin needs
Factors like stress, activity, and weight changes can all affect your insulin requirements over time.
Tight blood sugar targets
Aiming for non-diabetic blood sugar levels increases the risk of frequent lows, as even small doses of insulin or activity can cause a sudden drop.
Tip: If you’re experiencing frequent lows, review your insulin dosing for meals and corrections to prevent recurring hypoglycemia.
Read more about adjusting insulin doses, weight loss, and exercise in the following articles:
- How to Improve Your A1c: The Complete Guide
- How to Find Your Formula for Insulin and Food Around Workouts
- How to Lose Weight With Type 1 Diabetes
Tips for treating low blood sugars
The “rule of 15” or “15-15 rule” (eating 15 grams of carbs and checking blood sugar after 15 minutes) is a common guideline, but managing hypoglycemia in real life can be more nuanced.
Have a glucagon kit
For severe lows, such when someone is unable to eat or unconscious, a glucagon kit can be life-saving.
Glucagon is a hormone that raises blood sugar by counteracting insulin. Both injectable and nasal spray forms are available.
Make sure your prescription is up to date, store the kit in an accessible place, and ensure others know where it is and how to use it.
If glucagon is unavailable or the people present don’t know how to administer it, they should call 911 immediately.
Wear a medical ID
People with diabetes, especially those using insulin, should carry a medical ID at all times.
In emergencies such as severe hypoglycemia or accidents, a medical ID provides essential information, including diabetes status, insulin use, and allergies.
Emergency personnel are trained to look for these IDs when a person is unable to communicate.
Medical IDs are typically worn as bracelets or necklaces and can be engraved with key health details, with some now offering USB drives to store full medical records.
Use fast-acting carbs
Avoid slow-digesting foods like chocolate bars; instead, choose quick-absorbing carbs such as glucose tabs, gummy candy, juice, or honey to raise blood glucose quickly.
Learn more in: How to Treat Lows as Quickly as Possible.
Treat with 5 to 15 grams of carbs
For mild lows (around 65 mg/dL), 5 grams may suffice. More severe lows (55 mg/dL and dropping) may need 15 grams or more depending on insulin levels. Be patient — check your meter before eating more to avoid overtreatment.
Read more in: What is Considered Low Blood Sugar?
Keep fast-acting carbs everywhere
Stock up on quick carbs in places like your nightstand, purse, car, or office to ensure you’re always prepared, especially in extreme temperatures where some foods might spoil.
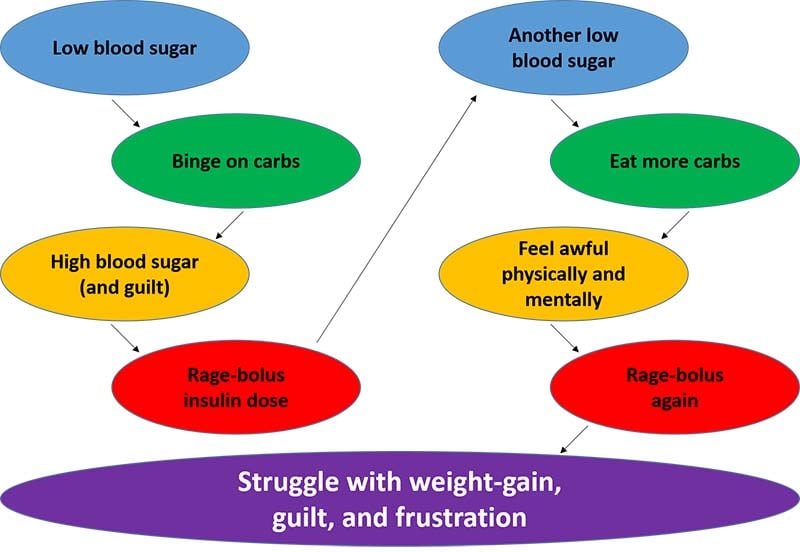
Avoid binge-eating
It’s common to overeat during lows, but this can cause a glucose spike, guilt, and the need for more insulin, which may lead to another low. Recognize this cycle from my book, “Emotional Eating with Diabetes,” and focus on healthier low treatments.
Navigating the complexities of low blood sugar
Low blood sugars can be a real challenge. For those taking insulin or other glucose-lowering medications, they’re often an inevitable part of diabetes management.
The best approach is to identify areas for adjustments to prevent lows and always have fast-acting carbohydrates on hand for treatment when they occur.
Did you find this article helpful? Click Yes or No below to let us know!





Carolyn Smith
I take Novolin N for many years and pretty much kept at good blood glucose levels, I eat an evenly balanced 2 meals spaced out 2 times a day. Got 4 units with breakfast and checked insulin 6 hrs. later and it was 62, what do i do? Do I skip a dose, just go down in units and to what? Scared of even taking 1 or 2 units. My weight has stayed the same but as i get older could i need less insulin? Thank you!
Christel Oerum
We can’t give dosing recommendations here on the website, that decision should be made in collaboration with your medical team. But if you consistently go low you need less insulin or more carbs. An occasional low blood sugar of 62 is probably nothing to worry about and you can treat it with juice or glucose tablets. The general guideline is 15-15 which means eat 15 grams of carbs, wait for 15-min and if you’re not back in range eat more carbs
Jeremy Cobble
Umm yes do you have a list where to purchase all these products I’m a late bloomer to diabetes and I’ve experienced lows I would rather avoid the subject if at all possible. I know it probably won’t be the last time but I could use a list of places to purchase these products and if any are close to me.
Christel Oerum
I’m glad this article was helpful. Which products specifically are you looking for?