To a non-diabetic, a low blood sugar sounds like a fun excuse to eat candy. For those of us with diabetes, low blood sugars are the exact opposite of fun.
Low blood sugars (also known as hypoglycemia) can interrupt business meetings, put you in danger while driving, turn a trip to the playground with your kids into a nightmare, and leave you feeling like a panicky, sweating mess.
In this article, we’ll look at the telltale symptoms of low blood sugar, the causes of low blood sugar, how to treat and manage lows, and how to prevent them from occurring as frequently.

What is low blood sugar?
In a non-diabetic body, blood sugar levels rarely dip below 70 mg/dL. Any lower and the body will begin to struggle to perform even the most basic tasks.
Your brain relies on a second-by-second delivery of glucose from your bloodstream in order to function — physically and mentally. Without enough glucose (a form of sugar) in your bloodstream, your brain and entire body will struggle to function.
Left untreated, low blood sugars can lead to seizures and death.
- Read more about “normal” blood sugar levels.
What are the symptoms of low blood sugar?
There are several telltale signs that your blood sugar has dropped below a safe level. The American Diabetes Association (ADA) lists the following as symptoms of low blood sugar:
- Feeling shaky
- Being nervous or anxious
- Sweating, chills, and clamminess
- Irritability or impatience
- Confusion
- Fast heartbeat
- Feeling lightheaded or dizzy
- Hunger
- Nausea
- Color draining from the skin (pallor)
- Feeling Sleepy
- Feeling weak or having no energy
- Blurred/impaired vision
- Tingling or numbness in the lips, tongue, or cheeks
- Headaches
- Coordination problems, clumsiness
- Nightmares or crying out during sleep
- Seizures
You may experience other symptoms beyond this list. For example, in my body, if I’m walking on a treadmill and my blood sugar is low, my thighs start to feel numb and tingly.
Everyone has their own classic symptoms of low blood sugar — figure out which symptoms you feel the soonest so you can catch lows sooner than later!
Hypoglycemia unawareness
For some people, especially those who have lived with diabetes for many decades, “hypoglycemia unawareness” can become a problem.
This means that your blood sugar could be low but your body no longer experiences the common symptoms of a low, putting you in greater danger of experiencing a seizure.
The ADA says it is possible to regain symptoms of low blood sugar, but it takes time and purposeful changes in how you approach diabetes management.
“It’s possible to get your early warning symptoms back by avoiding any, even mild, hypoglycemia for several weeks,” explains the ADA. “This helps your body re-learn how to react to low blood glucose levels. This may mean increasing your target blood glucose level (a new target that needs to be worked out with your diabetes care team). It may even result in a higher A1C level, but regaining the ability to feel symptoms of lows is worth the temporary rise in blood glucose levels.”
Reversing “hypoglycemia unawareness” is possible for many
While it isn’t remarkably common, it is an issue for some people with diabetes. There are a few things someone with clear “hypoglycemia unawareness” can do to keep themselves safe.
First, use a continuous glucose monitor (CGM). CGMs are ideal for people who don’t experience normal symptoms of low blood sugar because they can alert you to oncoming lows, helping you prevent them from occurring or from dropping as severely. CGMs allow you to set “low alerts” to levels like 90 mg/dL or 110 mg/dL — wherever you feel safest.
Secondly, aim for a higher target range. If you know you have “hypoglycemia unawareness,” it’s critical that you raise your target blood sugar range at least slightly. Instead of aiming for 90 mg/dL when dosing insulin for meals and correcting highs, talk to your diabetes healthcare team about aiming for 100 mg/dL or 110 mg/dL, etc. This will reduce the risk of low blood sugars by keeping your blood sugar slightly above that thin line between “normal” and “low.”
Symptoms of low blood sugar when you aren’t actually low…
For people with diabetes whose blood sugar levels have been consistently high for an extended period of time, including those with A1cs above 8 percent and those struggling with diabulimia, it is possible for your body to acclimate to high blood sugar levels.
This means that when your blood sugar does come down, your body might show symptoms of being low even when it’s just in a healthier range.
Reversing this issue is possible.
First, if you are currently struggling with diabulimia, please reach out to WeAreDiabetes or your healthcare team for support and guidance on working towards recovery.
Secondly, explain to your CDE what’s going on — that you’re experiencing symptoms a low when you’re not low — and that you’re fully committed to improving your blood sugar levels so you can feel good at healthier blood sugar ranges.
But this means your body needs time to acclimate, too. You’d work with your CDE on aiming for a target blood sugar that’s lower than the higher range you’ve been sitting at, but not as low as “normal” blood sugar targets.
This gives your body a chance to gradually — over the course of weeks or months — reacclimate to healthier blood sugar levels without triggering false symptoms of low blood sugar.
What causes low blood sugar?
In people with type 1 and type 2 diabetes, low blood sugars are generally caused by an imbalance of food, activity, and insulin — or other diabetes medications that lower blood sugar.
Exercising without adjusting insulin doses and carbs
Going for a walk after lunch, for example, can cause a severe low blood sugar if you took your full dose of insulin for your lunch. The addition of the walk increases the rate at which your body is burning up the glucose from the meal you ate, causing a low blood sugar.
TIP: Learn, learn, learn, and study, study, study how the body reacts to different types of exercise in Christel Oerum’s “Fit with Diabetes” guide, or Sheri Colberg’s “Diabetic Athlete’s Handbook.”
Dosing insulin for tricky carbohydrate estimates
Taking 3 units of insulin for a medium-sized apple when you may have only needed 2 is another example of the simplest way people with diabetes can experience low blood sugars while doing our best to manage our blood sugars.
TIP: Use CalorieKing.com to doublecheck your carb-counts, and keep a little notebook of the insulin doses you used for meals you eat often!
Weight-loss increasing sensitivity to insulin
Losing 5 pounds can result in the body eventually needing less insulin, but a person with diabetes only knows it’s time to reduce their insulin doses when they start to experience frequent low blood sugars.
TIP: Chances are, your body needs a reduction of at least 1 to 3 units in your overall background insulin needs or more for those losing larger amounts of body fat. Talk to your CDE about performing some basal testing and carb-ratio testing to be sure your current insulin doses are accurate! (Or read Gary Scheiner’s Think Like a Pancreas!)
Insulin needs changing due to other factors
Your insulin needs can change throughout your entire life due to changes in stress, activity level, body weight, growth spurts, etc. If you never fine-tune and adjust your insulin doses, you’re bound to experience more high or low blood sugars.
Tight blood sugar targets
Aiming for healthy non-diabetic blood sugar ranges means its far more likely you’ll experience low blood sugars because the line between “normal” and “low” blood sugars is a very thin line. Just the slightest bit too much insulin or activity, and your blood sugar is suddenly too low.
TIP: When aiming to improve your A1c, the first priority is to prevent and avoid recurring low blood sugars. If you’re constantly going low, it’s time to take a closer look at the doses you’re using for meals and corrections. If taking 2 units of insulin when your blood sugar is 200 mg/dL constantly sends you down to 50 mg/dL, that’s a very clear sign that you need far less insulin for your correction doses. Take good notes and pinpoint areas where you can make adjustments.
Especially if you’re taking insulin — and if you take non-insulin medications that lower blood sugar — low blood sugars are something you will be constantly working to avoid, treat, and endure.
Read more about adjusting insulin doses, weight-loss, and exercise:
- How to Improve Your A1C
- Fit with Diabetes Guide.
- Find Your Insulin Formula for Exercise
- How to Lose Weight with Diabetes
Tips for treating low blood sugars
While we’re often told that all low blood sugars should be treated with the “rule of 15” (eat 15 grams of carbohydrates and check again after 15 minutes), real life with diabetes isn’t this simple. Let’s take a closer look at how to treat low blood sugars.
Make sure you have a glucagon kit
For the very worst lows — when you’re unconscious or when you’re sick and you can’t keep food down — a glucagon kit can save your life. If you don’t have one, or the one you have is expired, ask your doctor for a new prescription. Keep it in somewhere in your house or at work or in your gym bag, and make sure others know where it is and how to use it!
Use fast-acting carbohydrates
If you treat your lows with a chocolate candy bar, the fat and protein in the bar are going to slow down the digestion of the carbohydrates. This means it’ll take longer for your blood sugar to come back up! Instead, choose fast-acting carbohydrates like glucose tabs, gummy candy, juice, dried fruit, jelly beans, Pixie Stix, honey, syrup, etc.
Treat with 5 to 15 grams of carbs and be patient
Some lows only require 5 grams of carbohydrates to bring you back up to a safe level. If you’re sitting steadily at 65 mg/dL, you likely don’t need a full 15 grams of carbs, because that might bring you back well above your target blood sugar range.
On the other hand, if you’re at 55 mg/dL and continuing to drop, you may need 15 grams of carbohydrate…and then more depending on the amount of insulin you have onboard and why you’re low.
Then, here’s the hardest part: sit on your hands and wait before eating anything else. If you are still low then you would treat with more carbs. (Do check with your meter because symptoms can last even when your blood sugar has come back up).
Always keep fast-acting carbs nearby…everywhere!
In your nightstand, in your purse, in your child’s diaper bag, in your car’s glove compartment, in the jacket you wear to walk the dogs, in your office desk, in your partner’s car. Everywhere!
Remember to choose fast-acting carbs. And if they’re going to be in a location that can get really cold or really hot, you need to think about whether that type of food will rot or melt or freeze. Fruit snacks and Gummy Life Savers and traditional glucose tabs are great for hot or cold locations.
Remind yourself: I am in control of how much food I eat to treat my lows.
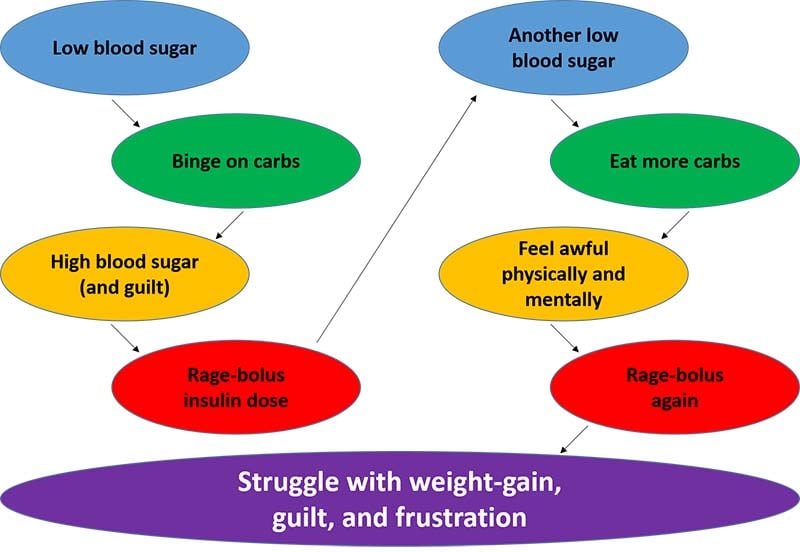
Binge-eating during low blood sugars is very common, but it can be a very destructive habit. The binge leads to a super spike in your blood sugar, which leads to guilt and shame and a “rage bolus” of insulin to bring it back down. And then that can lead to another low!
Is this a common issue for you? Ask yourself: is the way I treat my low blood sugars healthy or harmful to my overall well-being?
Here’s a simple look at the binge-eating cycle around low blood sugars from my book, Emotional Eating with Diabetes:
Low blood sugars are a real pain. For those of us taking insulin and other meds that lower blood sugar levels (like Metformin), they’re also an inevitable part of diabetes management.
The best we can do is pinpoint areas to make adjustments to prevent them, and always, always, always have fast-acting carbohydrates nearby to treat lows when they happen.

Carolyn Smith
I take Novolin N for many years and pretty much kept at good blood glucose levels, I eat an evenly balanced 2 meals spaced out 2 times a day. Got 4 units with breakfast and checked insulin 6 hrs. later and it was 62, what do i do? Do I skip a dose, just go down in units and to what? Scared of even taking 1 or 2 units. My weight has stayed the same but as i get older could i need less insulin? Thank you!
Christel Oerum
We can’t give dosing recommendations here on the website, that decision should be made in collaboration with your medical team. But if you consistently go low you need less insulin or more carbs. An occasional low blood sugar of 62 is probably nothing to worry about and you can treat it with juice or glucose tablets. The general guideline is 15-15 which means eat 15 grams of carbs, wait for 15-min and if you’re not back in range eat more carbs
Jeremy Cobble
Umm yes do you have a list where to purchase all these products I’m a late bloomer to diabetes and I’ve experienced lows I would rather avoid the subject if at all possible. I know it probably won’t be the last time but I could use a list of places to purchase these products and if any are close to me.
Christel Oerum
I’m glad this article was helpful. Which products specifically are you looking for?