Approximately 37 million Americans live with some form of diabetes, and between 90-95% of those who have it have type 2 diabetes.
Estimates vary, but about 1 in 3 people with diabetes require insulin to manage their condition.
The longer you have type 2 diabetes, the more likely you are to need insulin to manage blood sugar levels.
This article will explore insulin for type 2 diabetes management, and what you need to know.
Can type 2 diabetes be treated with insulin?
Yes. It is relatively common for people with type 2 diabetes to use insulin to manage their blood sugar levels.
Not everyone with type 2 diabetes gets put on insulin right at their diagnosis.
However, your doctor will likely suggest it if you struggle to keep your blood sugars down with exercise, diet, and oral medication alone.
This is not a bad thing, and there is no shame in needing insulin to manage your type 2 diabetes!
People with type 2 diabetes can be on many different types of insulin regimens. Some people may only require a little insulin, whereas others may require intensive insulin therapy.
The latter often includes using an insulin pump or taking insulin injections for every meal of the day.
When is the right time to go on insulin?
This is a very personal decision and is made between you and your doctor.
However, people with type 2 diabetes are usually referred to insulin treatment when diet and exercise alone, or even oral diabetes medications, are no longer keeping blood sugar levels within a healthy range.
According to the CDC, a healthy blood sugar range for someone with type 2 diabetes before a meal is between 80-130 mg/dL, and less than 180 mg/dL two hours after a meal.
However, your individual target blood sugars may vary.
Let your doctor know if you start to notice that your blood sugars spike after meals, are high when you wake up, and diet, exercise, and oral medications aren’t helping.
Going on insulin not only improves your blood sugar levels but helps prevent diabetes complications and extend your life expectancy as well.
Once your blood sugars are under better control, you’ll feel better and have more energy.
What are the different types of insulin?
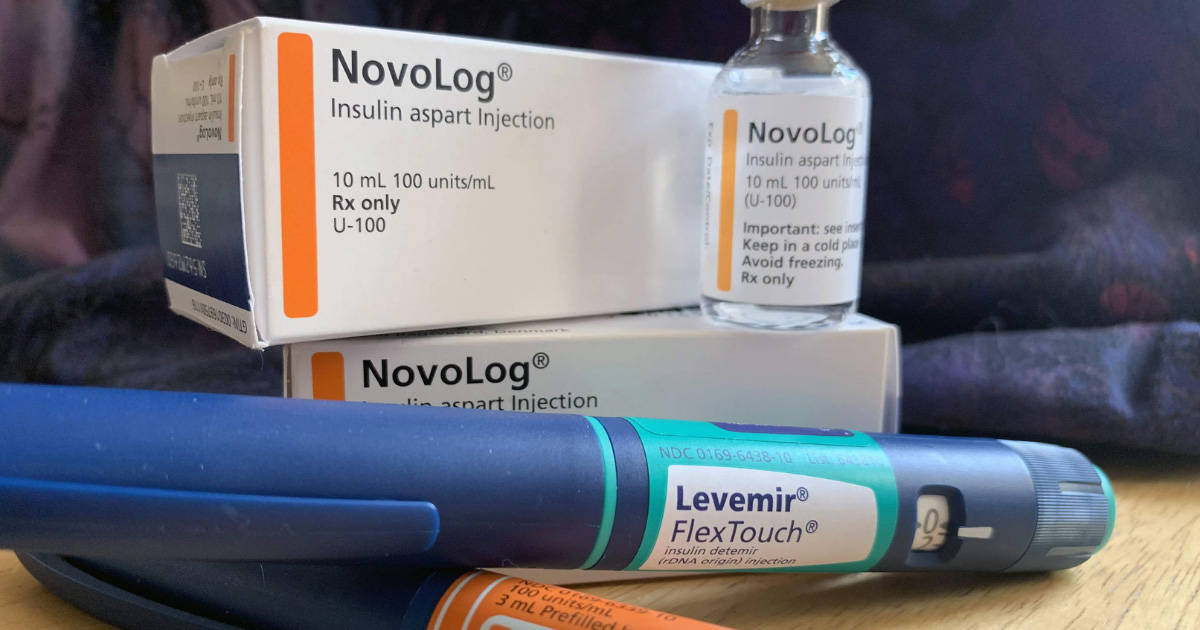
There are many brands of insulin, but there are fewer types.
The general types of insulin include:
Long, ultra-long, and intermediate-acting insulins
Longer-lasting insulins like these are necessary as background insulin for the body.
Even when you’re not eating, the body requires insulin for critical cell functions. This is because the liver naturally releases glucose.
Even without food, these insulins help the body combat high blood sugar levels throughout the day.
These types of insulin include:
- Intermediate-acting NPH (Humulin N, Novolin N, Novolin ReliOn Insulin N, which are more intermediate, and last between 4-12 hours)
- Long-acting detemir (Levemir, which is usually administered once or twice per day)
- Long-acting glargine (Lantus and Toujeo, which can be administered once or twice per day)
- Ultra-long-acting degludec (Tresiba, administered once daily or even every other day)
These longer-acting insulins can be taken with or without food, and usually any time of the day. The key is to remember to take the injection at the same time each day.
These are typically referred to as “basal” insulins.
Rapid, ultra-rapid, and short-acting insulins
Often, short-acting, rapid, and ultra-rapid insulins are necessary for people who are on intensive insulin regimens.
Similar to what someone with type 1 diabetes does, you’ll take more than one shot per day, often with every meal.
These faster-acting insulins usually need to be administered before you eat. There are a few exceptions, such as:
- It is recommended that children dose after they eat because they usually don’t finish all of their food.
- If you’re on a ketogenic diet with few carbs, you might be advised to dose after meals to prevent low blood sugar levels.
If you’re on a set regimen of Regular insulin, you’ll administer your dose at very specific times of the day. You’ll also need to eat according to your insulin regimen.
The newer versions of rapid-acting insulin work the other way around. You administer insulin to match the carbohydrates that you think you’ll eat.
Talk with your doctor about the appropriate timing of doses for your insulin before meals.
Examples of short-acting insulins include Regular (Humulin R, Novolin R, Myxredlin, ReliOn R).
Rapid-acting insulins include glulisine (Apidra) and lispro (Humalog and Admelog), and aspart (Novolog), which you’ll dose 15-20 minutes before eating a meal.
There is also Afrezza, which is inhalable and works within about 30 minutes of taking it.
Ultra-rapid-acting insulins are the newest and work the fastest.
People report being able to eat food within 5 minutes of injecting these medications, which include aspart (Fiasp) and lispro (Lyumjev).
These are typically referred to as “bolus” insulins.
What are the delivery options for insulin?
Except for inhalable insulin Afrezza, insulin must be injected subcutaneously (which means under the skin.)
You may either choose to use regular syringes or opt for an insulin pen. Many people find the latter to be more subtle when dosing in public. Plus, the risk of shattering an insulin vial is diminished.
Rapid-acting insulins taken with an insulin pump can sometimes replace the combination of longer and shorter-acting insulins.
Insulin pumps push steady micro-doses of rapid-acting insulin into your body via a thin tube continuously throughout the day and during mealtimes.
There are many different kinds of insulin pumps available, including Insulet’s Omnipid, which is tubeless and uses Bluetooth technology for all dosing.
Talk with your doctor to see what kind of insulin therapy they recommend for you.
Tips for administering insulin
Your doctor or a certified diabetes educator (CDE) will walk you through how to properly give insulin injections via a syringe or insulin pen.
If you’re on an insulin pump, you will most likely need to complete a full training for dosing insulin.
Ask your doctor what their recommendations are should you choose to use inhalable Afrezza.
These tips can help you when you’re first starting out on injectable insulin therapy:
- Always clean the injection site with isopropyl rubbing alcohol before injecting insulin
- Always use a clean syringe, and dispose of it after one use
- Dispose of all sharps in a puncture-proof container, like a sharps container or empty milk jug. Once this is full, it can be dropped off at a medical facility for proper processing and disposal.
- Insulin is best absorbed in areas where you can pinch about an inch of fat. Areas include the stomach, hips, thighs, arms, and legs.
- Make sure to rotate injection sites to avoid the development of scar tissue
- Insulin is best injected at a 90-degree angle, although talk with your doctor to see what angle they recommend for you
- Always check your insulin expiration dates and do not use expired insulin
What are the downsides to insulin therapy?
While insulin therapy is a great option for many people, there are some downsides and side effects that you’ll need to keep in mind:
- Insulin is expensive, especially in the United States, and without insurance, it can cost around $400 per vial. Some people with diabetes may require as much as one vial per week (there are typically 1,000 units in a vial.)
- Insulin increases your risk for severe hypoglycemia. Always carry glucose or low snacks with you, and ask your doctor for a prescription of Glucagon to treat severe low blood sugars in an emergency.
- Insulin itself doesn’t cause weight gain. However, many people will gain weight as their high blood sugar levels return to normal. This is healthy!
- Injections can hurt, and you may experience pain, redness, or swelling at the injection site
Conclusion
The decision to go on insulin therapy can be a difficult one to make but is best if the decision is made between you and your doctor.
If you’re struggling to manage your blood sugar levels with diet, exercise, and existing medications alone, insulin therapy can be a great and effective way to lower blood sugar levels and improve your health.
However, insulin therapy can be demanding and requires a lot of attention to detail.
Insulin therapy may increase your risk for dangerously low blood sugar levels, so be aware of that.
Additionally, insulin therapy can be expensive, and you may experience side effects including modest weight gain, and pain, redness, and swelling at the injection site.
It’s important that your doctor is aware of your dosing decisions because your insulin needs may change and vary over time.
When you choose an insulin regimen that supports your lifestyle and health goals, it can help prevent diabetes complications and improve your quality of life.



