Victoza is a prescription medication used to manage blood sugar levels in adults and children ages 10 and up with type 2 diabetes.
Key Facts
- Victoza stimulates insulin production, slows digestion, and reduces appetite, improving blood sugar and helping with weight loss.
- It lowers the risk of heart attack, stroke, and death in people with diabetes and heart disease.
- Common side effects include nausea, diarrhea, and vomiting while serious risks include thyroid cancer and kidney issues.
Table of Contents
- What is Victoza?
- How does it work?
- What are the benefits of taking Victoza?
- Why would you be prescribed Victoza?
- What are the side effects?
- What are the typical doses?
- What is the maximum daily dose?
- What happens if you take too much Victoza?
- Can I miss a dose?
- How do I inject Victoza?
- Who shouldn’t take Victoza?
- How do I stop taking Victoza?
- Can Victoza replace insulin?
- Can I take Victoza with other diabetes medications?
- Does Victoza need to be refrigerated?
- What does it cost?
- How do I get a prescription?
What is Victoza?
Victoza is an injectable drug approved by the U.S. Food and Drug Administration (FDA) for the management of blood sugar levels in type 2 diabetes.
It belongs to the glucagon-like peptide-1 (GLP-1) receptor agonist drug class, with its main ingredient being liraglutide.
Victoza is similar to medications such as Trulicity (dulaglutide), Ozempic (semaglutide), and Mounjaro (tirzepatide). It is administered subcutaneously (under the skin) once daily and can be taken alongside insulin or other diabetes medications.
How does it work?
Victoza helps to lower blood sugar in several ways. It stimulates insulin production from the pancreas, which helps prevent blood sugar spikes after meals, slows digestion, and suppresses appetite.
Additionally, it inhibits the liver from producing glucagon, thereby increasing insulin sensitivity and preventing blood sugar spikes.
When taken consistently, along with a healthy diet and increased physical activity, Victoza lowers blood sugar and A1c levels (a measure of glucose control over the previous 2 to 3 months), helping many people maintain a healthy weight.
What are the benefits of taking Victoza?
In clinical studies, people with diabetes who took Victoza experienced lower blood sugar levels, especially after meals.
Additionally, many people not only avoid weight gain while taking Victoza, but they also lose weight.
In a double-blind study involving people with diabetes, high blood pressure, high cholesterol, or obesity, Victoza combined with lifestyle counseling resulted in an average weight loss of 8.9 to 13.3 pounds, which was sustainable for over a year.
That said, not everyone in clinical studies lost weight while taking this medication — some even gained weight.
If weight loss is part of your diabetes management plan, talk to your healthcare provider about the best treatment options for you.
Victoza has also proven protective against heart attack, stroke, and premature death in people with diabetes and pre-existing heart disease.
Why would you be prescribed Victoza?
Victoza may be prescribed if you have type 2 diabetes, are experiencing insulin resistance, or are otherwise dealing with difficulties managing your blood sugar levels.
For example, occasionally, people without type 2 diabetes, such as those with type 1 diabetes or prediabetes, may be prescribed Victoza to help manage insulin resistance.
Additionally, people with existing heart disease may be prescribed Victoza due to its cardiovascular benefits. The medication is also sometimes prescribed off-label as a weight-loss medication for those facing challenges in maintaining or losing weight.
Always take Victoza only if prescribed by your doctor and under their guidance.
What are the side effects?
Common side effects include:
- Nausea
- Diarrhea
- Vomiting
- Decreased appetite
- Indigestion
- Constipation
- Weight loss
- Low blood sugar (particularly if you’re on insulin therapy)
Rare but serious side effects may include:
- Severe allergic reactions
- Impaired kidney function
- Gallbladder problems
- Medullary thyroid carcinoma (MTC)
Do not take Victoza if you have a personal or family history of MTC, multiple endocrine neoplasia, or if you are allergic to liraglutide.
The FDA has issued a black box warning for an increased risk of thyroid cancer with Victoza.
Learn more in: Victoza Side Effects: What You Need to Know.
What are the typical doses?
There is no single typical dose; it varies based on your health history, goals, lifestyle, and insulin resistance.
However, most people start with 0.6 milligrams (mg) once daily. After one week, if you’re not experiencing significant side effects, your doctor may increase the dose to 1.2 mg daily as a maintenance dose.
If insulin resistance and high blood sugar levels remain after a few weeks at 1.2 mg, your doctor may further increase the dose to 1.8 mg daily.
See more in: Victoza Dosing: How Much Should You Take?
What is the maximum daily dose?
The maximum daily dose of Victoza is 1.8 mg, taken once daily. It’s important to never exceed the prescribed dose.
What happens if you take too much Victoza?
Accidentally taking too much Victoza can result in severe side effects like nausea, vomiting, and diarrhea, which may lead to dehydration.
It can also cause dangerously low blood sugar levels (hypoglycemia), especially if you’re taking insulin.
If you experience low blood sugar and cannot keep food or drink down due to nausea, this is a medical emergency that could be life-threatening if not treated promptly. If you suspect an overdose, call 911 and seek emergency medical assistance immediately.
Can I miss a dose?
If you miss a dose, don’t worry — you won’t experience increased insulin resistance, higher blood sugars, or weight gain from missing a day or two.
However, it’s important to take your medication consistently for the best results.
If you’re within 12 hours of the missed dose, you can still take it. If more than 13 hours have passed, skip the missed dose and take your next dose as scheduled the following day.
Never take two doses within the same 12-hour period, and aim to take your injection at the same time each day, such as at breakfast.
How do I inject Victoza?
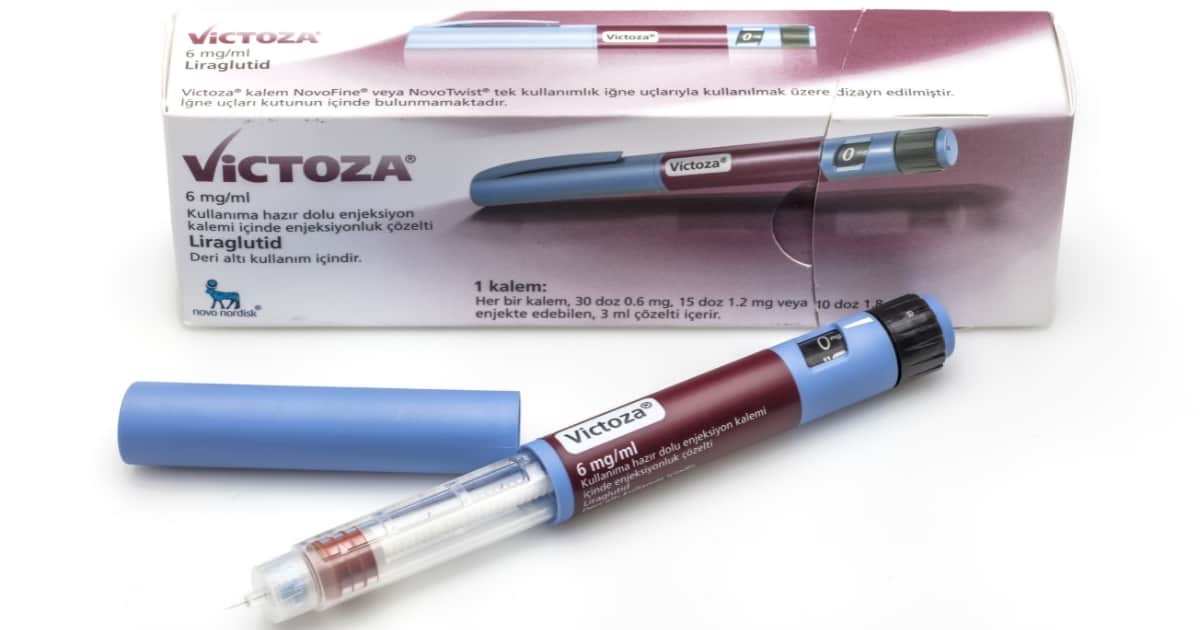
Victoza comes in a pen form and is injected subcutaneously (under the skin).
To inject, position the pen perpendicular to a fatty area of your body, such as your upper arms, thighs, or stomach.
Clean the area with an alcohol swab before injecting, and always use a new pen needle for each dose.
Dial your prescribed dose, pinch an inch of skin, insert the needle, and press the top of the pen to release the medication.
Hold the needle in place for about 10 seconds to ensure all the medication is delivered.
Afterward, twist off the needle and dispose of it in a sharps container. Finally, wipe away any excess medication or blood with another alcohol swab.
The medicine can be taken at any time of day, with or without food. To help you remember to take the medication, it’s best to get into a routine and take it at the same time each day.
To avoid injecting into the same spot too often, rotate your injection site to a different area each time.
Who shouldn’t take Victoza?
Victoza should only be taken if it has been prescribed to you by a doctor. It is FDA-approved only for people with type 2 diabetes.
If you do not have type 2 diabetes or haven’t been prescribed Victoza, do not take it.
Additionally, GLP-1 agonists are not recommended for those who are pregnant, planning to become pregnant, or breastfeeding.
Do not use Victoza if you are allergic to its active ingredient, liraglutide, or if you or any of your family members have a history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN 2).
If you have chronic kidney disease (CKD) or gastroparesis (a condition in which stomach emptying is delayed), consult your doctor before starting Victoza, as it can worsen these conditions.
How do I stop taking Victoza?
There are various reasons you might want to stop taking Victoza, such as experiencing adverse side effects.
However, it’s not recommended to stop taking the drug abruptly, as this can lead to increased insulin resistance, higher blood sugar levels, and weight gain, which can be harmful to your health.
If you wish to stop taking Victoza, consult your doctor first. They may suggest gradually reducing your dose over several weeks to prevent adverse effects. Your doctor might also recommend an alternative medication that better suits your needs.
Can Victoza replace insulin?
No, Victoza and other GLP-1 agonists are not insulin and cannot replace the need for insulin.
You should continue taking your prescribed insulin unless your doctor advises otherwise. While Victoza may help reduce the amount of insulin you need over time, it will not completely eliminate your need for insulin.
Can I take Victoza with other diabetes medications?
Yes, but it depends on the specific medications.
Victoza can be taken with insulin, metformin, and other medications used to manage conditions like high blood pressure, high cholesterol, and heart disease.
However, do not combine Victoza with other GLP-1 agonists, such as Ozempic (semaglutide), Mounjaro (tirzepatide), or Trulicity (dulaglutide).
Be sure to inform your doctor about all the medications you are currently taking before starting Victoza.
Does Victoza need to be refrigerated?
Yes, Victoza should be stored in the refrigerator between 36°F and 46°F (2°C and 8°C). After opening, it can be used for up to 56 days. Never freeze it or expose it to extreme heat.
What does it cost?
The amount you’ll pay each month, known as your co-pay, varies depending on your insurance plan. To determine your specific co-pay, use your prescription or medical card and use the Victoza coverage and co-pay calculator.
Victoza is widely covered by major health plans, including Medicare and Medicaid. If you have any questions regarding coverage or co-pay costs, you can contact Novo Nordisk support at 1-877-4VICTOZA (1-877-484-2869).
For those who qualify, the Patient Assistance Program (PAP) offers free medication. To learn more about this program, call Novo Nordisk’s PAP toll-free at 1-866-310-7549.
How do I get a prescription?
You may qualify for a prescription if you:
- Have type 2 diabetes and are struggling with insulin resistance.
- Have prediabetes or type 1 diabetes and are dealing with insulin resistance and related weight gain.
- Want to lose weight but do not have diabetes. In this case, you may be eligible for other FDA-approved weight loss treatments, such as Wegovy or Zepbound, which might have fewer side effects.
If you’re interested in taking Victoza, talk with your doctor to see if it’s the right option for you.
Did you find this article helpful? Click Yes or No below to let us know!






pubrica
Great breakdown on Victoza—appreciate how clearly you’ve outlined both the benefits and the side effects. As someone involved in medical writing and clinical research communications, I find it crucial that complex drug information like this is made accessible to the general public. For researchers or healthcare professionals working on similar topics, especially those looking to amplify the visibility of their findings, services like Pubrica’s research impact solutions can be incredibly valuable. From scientific infographics to simplified summaries and press-ready abstracts, they help ensure your research doesn’t just get published—it gets noticed. Thanks again for the helpful read!