This post may contain affiliate links. Please read our disclosure.
As people with diabetes, we are often told that having a low A1c is an important goal in our diabetes management. But do you know why?
Do you know what a good A1c target is, how to lower your A1c, and how quickly you can lower your A1c safely?
These are the questions I will answer in this comprehensive guide on what A1c is, how to lower your A1c, and why achieving a low A1c isn’t the only (or necessarily the best) goal when it comes to diabetes management.
Table of Contents
- What is A1c?
- How to test your A1c
- Why you should care about your A1c
- How to lower your A1c
- How quickly can you lower your A1c?
- Why you shouldn’t lower your A1c too quickly
- Can your A1c be too low?
- What is a good A1c target
- A1c vs. time-in-range
- Final thoughts: My perspective on A1c as a person living with diabetes
What is A1c?
A1c, also known as hemoglobin A1c, HbA1c, glycated hemoglobin, or glycohemoglobin, is a blood test that measures your average blood sugar over the last 2 to 3 months.
It’s not an “even average,” but rather a weighted average, where your blood sugar levels over the last few weeks count a little more than your blood sugar levels from 2 to 3 months ago.
According to the National Institute of Diabetes & Digestive & Kidney Diseases (NIDDK):
“The A1c test is based on the attachment of glucose to hemoglobin, the protein in red blood cells that carries oxygen.
In the body, red blood cells are constantly forming and dying, but typically they live for about three months. Thus, the A1c test reflects the average of a person’s blood glucose levels over the past three months.
The A1c test result is reported as a percentage. The higher the percentage, the higher a person’s blood glucose levels have been. A normal A1c level is below 5.7 percent.”
NIDDK
It’s important to note here that the term “normal A1c level” in this context refers to people without diabetes. I will get back to what a “normal A1c level” is for people living with diabetes below.
How to test your A1c
Your doctor or endocrinologist should test your A1c regularly (typically every 3 to 6 months). The doctor simply pricks your finger (or earlobe tip, if you prefer) and takes a tiny blood sample.
If the doctor’s office has an A1c kit, you should get your result before your consultation is over. (Some offices, however, will send the sample to a lab for processing.)
You can also buy home A1c kits (no prescription required) and do the test yourself. Home A1c kits can be useful if you go for more than 3 months between doctor visits and want to keep an eye on how your A1c is trending yourself.
The home kits are generally accurate within plus/minus 0.5 percentage points, which is more than good enough to give you a trustworthy result.
The downside of the home kits is that they require a larger amount of blood (generally, several large drops) than a regular blood sugar check, and if you don’t apply enough blood, you’ll get an error message and will have lost a test strip.
You can find home test kits on Amazon and in some pharmacies.
Read more in: How to Measure Your A1c at Home.
Why you should care about your A1c
Multiple significant studies have shown that high average blood sugars increase the risk of diabetes-related complications. Lowering your A1c to the recommended range will reduce the risk of diabetes-related complications significantly.
According to the landmark Diabetes Control and Complications Trial (DCCT) and the follow-up study called the Epidemiology of Diabetes Interventions and Complications (EDIC), in people who used intensive treatment to keep their A1c at the target level:
- Eye disease risk was reduced by 76 percent
- Kidney disease risk was reduced by 50 percent
- Nerve disease risk was reduced by 60 percent
- Any cardiovascular disease event risk was reduced by 42 percent
- Nonfatal heart attack, stroke, or risk of death from cardiovascular causes was reduced by 57 percent
Achieving an A1c in the recommended range is, therefore, one of the most important things you can do to improve your long-term health when you live with diabetes.
However, the closer you get to the recommended A1c target, the less benefit you will get from lowering your A1c further. For example, taking your A1c from 12.0 percent to 11.0 percent makes a big difference, while lowering your A1c from 7.0 percent to 6.0 percent provides a much smaller benefit.
In fact, lowering your A1c too much may not be a good idea if it means that you increase how often you experience hypoglycemia (low blood sugar).
I will explain why a measure known as “time-in-range” (TIR) is just as important as a low A1c later in this guide.
How to lower your A1c
Now that you have a thorough understanding of A1c, as well as why looking at your A1c in isolation isn’t optimal, the obvious question is:
How do you lower your A1c while improving or maintaining your time-in-range?
I will cover the four most important things you can do below, but it’s always recommended that you start by having a conversation with your medical team before making changes to your diabetes management.
Identify the main “pain points”
Whether you are largely self-managing your diabetes or working closely with your medical team, the first step should always be to try to identify the main “pain points,” or reasons why your A1c is higher than you’d like. The only real way of doing this is by tracking your blood sugars very closely.
If you wear a continuous glucose monitor (CGM), you can look at your 7-day, 30-day, and 90-day blood sugar data to see if you can spot any trends.
For example, you might find that you are running high from 1 a.m. to 5 a.m. every night, every morning (as in the dawn phenomenon, an early-morning increase in glucose level), or every day after meals. Or perhaps you always go low after exercise. We all have different blood sugar patterns.
It’s also very possible that you simply are running your blood sugar a little too high all the time and could benefit from adjusting your diabetes medication.
Identifying patterns like that makes it possible to pinpoint areas of potential improvement so you can start making a plan for how to limit your high and low blood sugars.
If you rely on manual blood sugar monitoring, it’s a little trickier, since most people don’t monitor every five minutes. In this case, you might try increasing how often you check for a while, and maybe even checking during the night if you wake up anyway.
Most meters allow you to download data to your computer, or you can upload the data to one of various app-based platforms. This can help you see the data in a more cohesive way so you can start looking for trends.
Create a plan for your diabetes management
Now that you have a better idea of what your “pain points” are, you can start making changes to your diabetes management.
Your doctor may suggest a different medication regime. For example, some people (regardless of their type of diabetes) are prescribed metformin to help with the dawn phenomenon. Others may need adjustments to insulin dosing or other medications.
If you’re using insulin and consistently have high blood sugars in the morning, getting your blood sugar fluctuations and A1c down might be as simple as adjusting your nighttime basal (background) insulin.
Or, if you run high every day after meals, your insulin-to-carb ratio might be off, and adjusting that could be what sets you on a path toward a lower A1c. Until you collect the data and do the analysis, you have no way of knowing this.
I want to make an important point here: increasing your diabetes medication is not a sign of failure. It’s often the best (and sometimes only) way to manage your blood sugar and bring down your A1c.
I adjust my insulin up and down all the time when I change my diet or exercise routine. The ability to adjust your medication is an important tool in your diabetes toolbox and something you should always discuss with your medical team.
Understand nutrition and adjust your diet
What you choose to eat and drink can have a major impact on your waistline, mood, and well-being, as well as your blood sugar levels.
All macronutrients (carbohydrates, proteins, and fats) can affect your blood sugar to some degree, so developing a good understanding of how they affect your blood sugar will enable you to be proactive and prevent blood sugar swings.
Carbohydrates (carbs)
Carbohydrates have the greatest impact on your blood sugar, which is why many people with diabetes can benefit from following a low- to medium-carb diet (or even a ketogenic diet). The fewer carbs you eat, the less insulin you need to take, which makes diabetes management easier.
However, you don’t have to follow a low-carb diet if it doesn’t work for you — physically or mentally.
As I wrote in my piece about which diet is best for people with diabetes, it is very possible to have great blood sugar management on a medium- (or even high-) carb diet, as long as you experiment, take notes, and learn to take the right amounts of insulin for the carbs you are eating.
It is very important to realize that we all react differently to carbs, so you have to find the diet and foods that are right for you.
As an example, people react very differently to carbs like oats or sweet potatoes. Some people can eat oats with only a small increase in blood sugar, while others see a quick spike.
By simply knowing this, people having difficulties with a certain type of carb can choose to reduce their consumption or cut it out of their diet altogether.
Protein and fats
While carbs affect blood sugar most significantly, protein and fat also have an impact. Some, like Dr. Sheri Colberg, PhD, one of the world’s leading voices on diabetes and exercise, even think that only looking at carbs when estimating blood sugar impact (and dosing insulin) is an outdated and inefficient way to pursue diabetes management.
In the opinion of these experts, you should focus more on total calories (read more about calorie counting and diabetes here).
The key thing to be aware of is that when protein and especially fat are consumed with carbohydrates, the energy from the meal will be released more slowly, which means that your blood sugars will be impacted more slowly as well.
While I don’t believe your diabetes management should completely dictate how you live your life and which diet you choose to follow, it can be worth evaluating which food choices make life easier for you.
By making a conscious choice of which type of nutrition plan to follow (the majority of the time), you can more easily establish healthy habits that will benefit not only your overall health but also your daily blood sugar levels, and thereby your A1c.
Increase activity (exercise)
While exercise is essential for building and maintaining good health and improving insulin sensitivity, it can be a double-edged sword if it constantly throws your blood sugars for a loop. Not only is that very frustrating, scary, and annoying, but it can also affect your A1c and time-in-range negatively.
The key is to understand how different types of exercise affect your blood sugar levels and, if you use insulin, to learn your formula for balancing insulin and food around workouts.
Cardio
Cardio, such as brisk walking, jogging, swimming, biking, or dancing, are all excellent types of exercise. As little as 20 to 30 minutes a day can make a significant difference when it comes to improving insulin resistance and managing blood sugar levels.
Not only does exercise reduce blood glucose during exercise, but it also improves your insulin sensitivity for hours after your workout, meaning that you need less insulin.
If you treat your diabetes with insulin, you will have to manage your insulin levels so you don’t experience exercise-induced hypoglycemia. This comes down to reducing your insulin significantly or consuming carbs before your workout.
For many people, it may not be necessary to “carb up” to do up to 60 minutes of steady-state cardio, but there can be situations in which reducing insulin before exercise can’t be done, so additional carbohydrates must be consumed.
And it’s also important to remember that different people react differently based on a variety of factors, such as insulin sensitivity, timing of their last insulin dose, and fitness levels, so this may not be the case for you.
Resistance training
Adding resistance training to your daily routine, such as free weights, weight machines, resistance bands, or bodyweight exercises, can be instrumental in increasing your insulin sensitivity and lowering your A1c.
Whereas cardio will lower blood sugar during exercise and potentially up to about 48 hours after exercise, resistance training can increase insulin sensitivity for much longer.
This is because muscles work as little “glucose tanks” and you’ll store more glucose in your muscles rather than sending it directly to your bloodstream. The more muscles you have, the better your insulin sensitivity.
Just be aware that some people will see a temporary increase in blood sugars during intense resistance training, rather than a decrease.
The reason for the increase in blood sugar is that the improved insulin sensitivity from exercising is surpassed by your body’s increased glucose production from the adrenaline released by the activity.
This adrenaline causes your liver to break down glycogen to create glucose, and your body is producing the glucose faster than you can use it.
For a detailed guide, read: How Resistance Training Affects Your Blood Sugar.
The shorter-term effects aside, because resistance training is so effective at increasing your insulin sensitivity, it’s a great way to lower your blood sugar and A1c consistently.
If you exercise regularly, the effect of exercising overlaps from one workout to the next, and you essentially achieve a permanent increase in insulin sensitivity. (Be sure to work with your healthcare team to adjust your treatment regimen to avoid lows from your improved insulin sensitivity.)
Maintain a healthy weight
If you are overweight, losing as little as 5 to 10 percent of your weight can help with various health markers, including A1c levels.
In one study, people with type 2 diabetes who lost this amount of weight reduced their A1c by an average of 0.5 percent.
How quickly can you lower your A1c?
Since the A1c test shows your glucose over the previous 2 to 3 months, it will take at least a few weeks of consistent dietary and exercise changes to see the results reflected in your A1c level.
The exact timeframe will vary based on individual factors such as the intensity of the changes and how your body responds.
(This is simply due to the long-term nature of the test — the improvements will reflect in your glucose much sooner.)
In this video, I explain how I lowered my A1c in 30 days by following 5 simple steps:
Why you shouldn’t lower your A1c too quickly
It can be a good idea to approach lowering your A1c with a bit of caution. Just as crash dieting isn’t healthy, there can be some serious health risks associated with lowering your A1c too quickly.
I turned to Dr. Anne Peters, MD, Director of the USC Clinical Diabetes Program, and Professor of Clinical Medicine Keck School of Medicine of USC, for an explanation:
“If you lower your A1c too quickly, many bad things can happen.
First, weight gain and total body swelling. Next, it can cause bleeding in the retina (back of the eyes) which can lead to blindness, and third, it can cause painful neuropathy [nerve damage] that never goes away.
It’s slightly different for newly diagnosed patients, but, in general, no one should try to go from an A1c of 10 percent to 6 percent quickly. Take slow steps. Wanting to get to a ‘low’ number very fast only causes harm.
Diabetes is a long-term disease, so slow steps to establish new habits that can last a lifetime are the way to go. Anything too sudden, and the body reacts badly.”
Dr. Anne peters
It’s important to work with your healthcare team to determine the best A1c goal for you and the appropriate timeline for working your way toward this target.
Can your A1c be too low?
As described above, the answer to this question depends almost entirely on how often you experience hypoglycemia. If you (almost) never experience hypoglycemia and your A1c is at target, this would suggest that your diabetes management is effective.
However, this doesn’t mean an extremely low A1c is always safe or desirable. Each person’s ideal A1c level can vary, and factors such as their risk of hypoglycemia unawareness, how long they have had diabetes, age, and overall health need to be considered.
Uncommonly, some people achieve A1c levels below 5.0 percent by following a very strict diabetes management and diet regimen and have almost no blood sugar fluctuations.
However, if you often experience hypoglycemia, that will result in an “artificially” low A1c reading because your hypoglycemia events are lowering your blood sugar average.
In that case, focusing on increasing time-in-range is much more important than further lowering your A1c. In fact, you may even benefit from a slightly higher A1c with fewer blood sugar fluctuations.
It’s also important to note that lowering your A1c below the generally recommended range of 6.0 to 7.0 percent hasn’t been proven to provide any health benefits. Therefore, a very low A1c shouldn’t be a goal in itself.
What is a good A1c target
Now that you have your A1c number, let’s look at what that number actually tells you. The American Diabetes Association has established the following guidelines
| A1c Level | What It Means |
| Less than 5.7 percent | Normal (minimal risk for type 2 diabetes) |
| 5.7 percent to 6.4 percent | “Prediabetes,” meaning at risk for developing type 2 diabetes |
| 6.5 percent or greater | Diagnosed diabetes |
This does NOT mean that you need an A1c of less than 5.7% if you’re living with diabetes. It means that if you do NOT live with diabetes, your A1c is expected to be below 5.7%.
There are different recommendations for what an appropriate A1c is for people living with diabetes.
I had a chance to ask Dr. Peters, as well as Gary Scheiner, MS, CDCES, owner and Clinical Director of Integrated Diabetes Services and author of Think Like a Pancreas, what their perspectives are on a good A1c target:
Dr. Peters:
“The A1c target should be whatever is best given the person’s clinical situation.
For athletes, too many lows can limit performance, for someone who is pregnant it should be less than 6.0 percent, for an older person the target should be higher.
I generally think an A1c target of 6.0 to 7.0 percent is ideal and data shows that going below 7.0 percent has fairly little impact on complications.
Basically, I’d rather see someone with an A1c of 6.9 percent and low blood sugar variability than an A1c of 6.2 percent with lots of variability.”
Dr. Anne Peters
Scheiner:
“A1c goals should be individualized based on the individual capabilities, risks, and prior experiences.
For example, we generally aim for very tight A1c levels during pregnancy and more conservative targets in young children and the elderly.
Someone with significant hypoglycemia unawareness and a history of severe lows should target a higher A1c than someone who can detect and manage their lows more effectively.
And certainly, someone who has been running A1cs in double digits for quite some time should not be targeting an A1c of 6.0 percent … better to set modest, realistic, achievable goals.”
Gary Scheiner
Read more about A1c in: What is a “Normal” HbA1c? and What is a Dangerous Level of A1c?
In their Standards of Care in Diabetes — 2024, the American Diabetes Association recommends an A1c target of below 7.0 percent for adults living with diabetes.
An A1c of 7.0 percent roughly translates to an average blood sugar of 154 mg/dL (8.6 mmol/L) as you can see from this conversion chart (eAG stands for “estimated average glucose”).
| A1c | eAG (mg/dL) | eAG (mmoL) |
| 5 percent | 97 | 5.4 |
| 6 percent | 126 | 7.0 |
| 7 percent | 154 | 8.6 |
| 8 percent | 183 | 10.2 |
| 9 percent | 212 | 11.8 |
| 10 percent | 240 | 13.3 |
| 11 percent | 269 | 14.9 |
| 12 percent | 298 | 16.5 |
| 13 percent | 326 | 18.1 |
| 14 percent | 355 | 19.7 |
Learn more about converting A1c to average glucose levels in: How to Translate Your A1c to a Blood Sugar Level.
A1c vs. time-in-range
A1c has long been considered the best measure of diabetes management because it was the most accurate tool for observing long-term blood sugar trends. This has changed with the introduction of continuous glucose monitoring (CGM).
By using a CGM, you can now get a very accurate picture of not only your average blood sugar, but your blood sugar fluctuations as well.
This makes it possible to track another key component of diabetes management: time-in-range.
Time-in-range refers to the percentage of time during which your blood sugar is within a specific range. To see why time-in-range is important, take a look at the three lines in the graph below.
All three lines show an average blood sugar of about 154 mg/dL (8.6 mmol/L, which equates to an estimated average A1c of about 7.0 percent) but with very different fluctuations. I think we would all prefer our blood sugar to follow line 3 rather than line 1.
Graph used with permission from diaTribe.
Some guidelines state that your blood sugar range should be set to 70 to 180 mg/dL (3.9 to 10 mmol/L), but you may find that to be too wide or narrow of a range for you.
According to this interview with several diabetes experts, most recommend that you spend less than 3 percent of the time below 70 mg/dL (3.9 mmol/L) and less than 1 percent of the time below 53 mg/dL (3 mmol/L). However, they also agree that the actual time spent in range needs to be individualized.
On average, the experts didn’t expect the general diabetes population to be in range more than 50 percent of the time at most, so talking about incremental improvement makes more sense than setting a fixed number.
How to measure time-in-range
If you wear a CGM, your time-in-range metrics should be listed when you download your data (as in the example from a Dexcom CGM below).
Some CGM devices offer alerts when glucose levels are predicted to enter or leave the target range, which can allow users to respond proactively and spend more time in range.
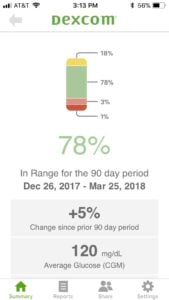
(Click to expand.)
If you don’t use a CGM, all you can do is look at your manual blood sugar measurements and pay attention to the amount of high and low blood sugar readings outside of your target range.
What’s an acceptable high and low is something you have to discuss with your medical team.
What is more important: a low A1c or a high time-in-range?
Ideally, you’d have an A1c below 7.0 percent accompanied by low blood sugar variability (high time-in-range). A good general guideline is:
- The higher your A1c, the more important it is to focus on getting it down.
- The lower your A1c, the more important time-in-range becomes.
If your A1c is below 6.0 to 7.0 percent, focusing on increasing your time-in-range will probably have a larger positive health impact than lowering your A1c further.
So, is A1c a bad way to gauge whether your diabetes management is on track? Not necessarily, but to quote Scheiner:
“I’ve never been a huge fan of using A1c to gauge the ‘quality’ of a person’s glucose control, simply because it represents an average … and an average can reflect lots of highs and lows rather than time spent within one’s target range.
However, it’s not something we can ignore either since there is a correlation between A1c and the risk of long-term complications.”
Gary Scheiner
Final thoughts: My perspective on A1c as a person living with diabetes
I have a very ambivalent relationship with my A1c myself. I’ve been living with type 1 diabetes for over 20 years, and my A1c is not something I think about in my daily life.
However, every 3-6 months when I see my endo, I get a little anxious because receiving your A1c can feel a lot like getting your diabetes report card.
And, quite honestly, that’s really silly. My A1c number doesn’t reflect what’s been going on in my life for the last 3 months. It doesn’t tell me how much effort I’ve put into managing my diabetes and it does not define me as a person. It’s a good source of information, nothing more.
Still, we tend to look at it and judge, good or bad, how we’ve done with our diabetes management. But we really shouldn’t!
That doesn’t mean that I think we shouldn’t get our A1c checked. I absolutely think we should, but we also need to understand what it means as well as why we should look beyond the A1c number. I hope this guide has given you the knowledge and tools to do so.


Lydia
A particularly excellent article. Thank you.
Penny Pritchett
I just want to thank you for such a intuitive message. My daughter of 16 years old was diagnosed with diabetes at 13% A1C and we didn’t even know. She went for pink infection and they ask her to urinate In a cup and that’s how we found out. We were devastated. So now we are on the road to recovery. And this article was so helpful. God bless you on your journey to educate people about this terrible disease. We got this and not gonna let this defeat us. Again. THANK YOU❤️
Amrit kambo
Hi Penny,
We also recently learned the same, our 16 years old daughter with Type 1.
I agree it is very heart breaking and devastating.
Melanie Winrow
Just to update you. Unsurprisingly the surgery was cancelled. I am devastated. The new doctors are referring me back to the diabetes team, which is what I wanted in the first place. Also he is asking if I can have an adjunct to help me get back in a level playing field. My sensor problem was down to APPLE. Nothing wrong with the sensor…but it cost me £500 to find that out. Hopefully I will get better news in 6 weeks when I go back. I will let you know. Have a wonderful day
Christel Oerum
I’m sorry to hear that… It all sounds very frustrating
Melanie
Just got a call from the hospital and I had to message you. After almost a year of cancelled surgeries, I got the call I yearned for … kind of. My wonderful pre-op nurse was AMAZING – she supported me every step of the way. She called and told me that she had good news. I have done it. I’ve reduced my HbA1c by over 40 points in 6 months. She then told me she is marking me safe for surgery. While I’m very slightly above what I’m supposed to be, she said that’s not my fault that. they changed it the wee before I managed to get the result I wanted. I had been told that as long as my sugar was 80 (it was 83 when they refused to do it …) I would be OK – then, 3 days before I did my last blood test, they lowered it further – to 64! I burst into tears – no way. could I do that.
But my pre-op nurse believed I could … as a result, I went all out, doing everything I could to reduce it further. She had a word with the anaesthesiologist who said, seeing such a big improvement, I CAN be marked safe for surgery. After ll by the time the surgery rolls around, I’ll be MUCH lower…
I spoke to the hospital today and they said there was an 18 month waiting list. It would be tough (especially as one of my consultants is apparently inhuman – there is no wiggle room. I CANNOT go over 9, no matter what I’m doing … as I’m walking a million steps in 92 days, I need my sugar to be at least high enough that I can do the walk without fearing hypos. I’m speaking to my favourite DSN next week so hopefully she’ll be able to support me – he told me just not to walk and I’d be a ‘nugget’ if I walked when my sugar was 6 or less. I know that … but 9 isn’t that much higher if you’re doing a long walk. “Well don’t have carbs, that’s all I can say.” What CAN I have then, if my sugar goes low? “Anything but carbs and sweets.” Sounds like I’m stuck with those revolting glucose tablets.
I WILL figure it out. I WILL continue walking – but I will keep my HbA1c down now. The guy I mentioned above dropped my insulin by 10 points (my background) and my sugars have started running MUCH higher. I’m panicking because I now have just 3 weeks to keep this in target. I’m going to speak to my favourite DSN and find out if there’s a ‘sweet spot’ where I can keep it low enough to help my bloods but not take so little that I’m running at 10 or higher in the morning. The guy wouldn’t listen. He told me never to worry if my HbA1c is high … BAD advice for a doctor to give!
Anyway, I just wanted to let you know that I’m having the surgery (now I’m having panic attacks, remembering the first one …) on 31st October!!! Can’t believe it.
Christel Oerum
Thank you for sharing. I hope you get your insulin to the level that’s needed and good luck with the surgery
Elizabeth James
Thank you so much for this article (difficult to read though it was because of the font – I’m severely sight impaired, nothing to do with my. diabetes but to do with the accident that triggered it). Most VI’s find it difficult to read a serif font/times new roman.
I found this SUPER helpful.
I rarely leave comments but … I’m in a mess. I got my A1c down to 5 points below target which astounded the hospital – but it meant I was doing too well so I was cut adrift with ZERO help. Can’t call my DSN – they made it quite clear she is not allowed to accept a call from me as I’m no longer a patient with poor control(!), can’t call my doctor – getting hold of her (or anyone else) is impossible; can’t call the DSN at the doctors as they said there is a 4 month waiting list to see her. Can’t call the hospital – they keep referring me back to my GP. So I’m alone on an endless sea.
The problem is … I HAVE to lower my A1c quickly if I want some surgery in 6 weeks … I’ve explained my GCM hasn’t been working for 2 months so I was unaware of my estimated A1c; I did request a recheck couple of days before. I am now walking 4 miles – sometimes 5 – a day, drinking water (which I LOATHE) – 6 glasses a day. I DREAD breakfast, dinner and tea time but I’m forcing myself to eat 3 times a day and I’ve vowed not to have a single ‘banned’ food or even any (or as few as I can manage without a hypo) carbs until the surgery. I know I’m going to feel rough. I also heard the comment (I had to get Siri to read it) saying it’s dangerous to lower it too quickly but I’m absolutely terrified of them cancelling this surgery. Long story behind my fear … I’m going to ask if I can get it to 71 or 72 – just two above what they want – it’s only 9 above it now – will they do it? I think if I’m willing to put all that work in – believe me, I’m getting sick of walking that far – now I’ve changed my routine is not as bad. but … it does drive me mad – they should meet me half way.
This article is incredibly helpful and reassuring to me – and it’s good to know that if I have to put my insulin up a little I’m not a failure. thank you so much.
Christel Oerum
Thank you for leaving a comment. I’m so sorry to hear that you’re not getting the support that you need, that’s disgraceful. It sounds like you’re doing everything in your power to reach your goal and I hope your surgery goes well. Even if your DSN won’t take your call, I wonder if the place where your surgery is due will. Maybe they can give you some clarity on how “on the money” you have to be with the A1c goal. And as for your CGM, try calling the manufacturer, they can often be quite helpful
Elizabeth James
Thank you. The hospital said they are reviewing the case and would make a decision on if the surgery can go ahead on the 26th. It’s now the 28th and I’ve heard NOTHING. I called, left messages … nothing. Now the stress is affecting my sugar and sending it into the stratosphere. As it is, I’m absolutely terrified of this surgery but I MUST have it.
I have changed doctors but they now say that I can’t see them until the day beforeth surgery. Can they find out if it’s been cancelled? No. I have to speak to them.
I have now SOLVED the problem with the sensor – took some doing. The manufacturers were blaming the phone company, who said it was the manufacturer (of course they did). Several people from Apple said I should just buy a new phone … as easy as that?! We know a LOT of people are having these issues but I went to John Lewis and explained. She got 6 phones out, loaded the app on ALL of them (easy to delete) and tested them on me. Only one (the SE) worked. I had to buy that for £500 – which is money I don’t have. At least I have a working sensor.
Thank you so much for your support and encouragement. Just having a reply from you makes me feel I’m not alone.
Have a wonderful weekend.
Christel Oerum
Keep fighting. Rooting for you
Peter
Hi, I am 39 and my a1c was 6.9 and I reduced it to 5.5 in 3 months and lost weight from 160 pounds to 149 pounds by walking or running. Did I do anything wrong?
Peter
Sorry it was from 160 pounds to 120 pound. Peter again here
cici
40 lbs in 3 months? How is that even possible? 90 days. Wouldn’t most doctors and trainers warn against losing weight too fast. Did you have surgical help?
Christel Oerum
Well done, sounds like you’re doing a lot of positive things for your health. Doesn’t sound like you did anything wrong, just remember to regularly check in with your doctor
Michael McCulloughllough
I’m 67, 6’2″ and 205 pounds. Since having my first A1c test in December 2021 revealed a 6.7. I wasn’t going to let diabetes dictate my life so it wasn’t difficult to accept that I was going to make some serious changes. My second A1c test in April 2022 was 6.3 and my most recent A1c last week was 6.0…..crossing back into prediabetes. I’m happy.
Honestly, it’s become a challenge now that see how I can control my health with little effort resulting in significant change. I’m gonna continue improving until I’m within high 5 range.
If I can do it, so can others.
Akshaya
Hii I have diabetes from 14 years…My Hba1c test was 12% before a month and I had my DNC before a month ..can you please tell me how it is connected with my pregnancy and how many percent should my A1c percentage be before I plan fr my next pregnancy
Christel Oerum
Below you’ll find a few articles discussing diabetes and pregnancy. Considerations vary a bit depending on what type of diabetes you live with and how it’s treated so choose the article that’s relevant for you
Pregnancy and Type 1 Diabetes: Type https://diabetesstrong.com/pregnancy-and-diabetes/
Pregnancy with Type 2 Diabetes: https://diabetesstrong.com/pregnancy-type-2-diabetes/
Gestational Diabetes: https://diabetesstrong.com/gestational-diabetes/
Lawrence Hutchinson
I am a 66 yo male, very active, 5 feet 9 inches and 155 pounds. Resting heart rate is in the low 40s and the cardiologist told me to decrease the amount I exercise. A1C has been in the range of 5.9 to 6.1 for several years. Fasting blood sugars run from 90-100 -while after eating blood sugars are 90-110. A year ago, I was put on carb restrictions of 200 gm per day. I dropped 10 pounds in a few weeks and was hungry all the time. I added more carbs and gained about 5 pounds back. Recently my A1C increased to 6.3. My primary care physician advised me to do nothing and re-check the A1C in one year. I am not comfortable with this. My father had diabetes and had a major stroke at age 62 and died of a presumed heart attack at 67. Please advise.
Christel Oerum
If you’re uncomfortable with your doctor’s advice, you could get a second opinion, or push back on your doctor and ask him/her what the recommendation is based on. You don’t mention your diagnosis but an A1C of 6.3% is indicative of pre-diabetes and to put that into context the American Diabetes Association states that the goal for most adults with diabetes is an A1C that is less than 7%