This post may contain affiliate links. Please read our disclosure.
As people with diabetes, we are often told that having an A1c in target is an important goal in our diabetes management. But do you know why?
Do you know what your A1c target is, how to lower your A1c if needed, and how quickly you can lower your A1c safely?
Key facts
- A1c reflects average blood sugar levels over 2 to 3 months and is associated with a person’s risk of diabetes-related complications.
- Regular A1c monitoring, through medical professionals or home kits, enables people to monitor and manage their diabetes more effectively.
- Maintaining an A1c within the recommended range significantly reduces the risk of complications such as eye, kidney, and nerve diseases, as well as cardiovascular events.
- While lowering A1c is important, focusing on “time-in-range” is equally important, especially for people with A1c levels between 6 to 7 percent, to maintain overall health and minimize hypoglycemia risks.
Table of Contents
- What is A1c?
- How to test your A1c
- Why you should care about your A1c
- How to lower your A1c
- How quickly can you lower your A1c?
- Why you shouldn’t lower your A1c too quickly
- Can your A1c be too low?
- What is a good A1c target?
- A1c vs. time-in-range
- Final thoughts: My perspective on A1c as a person living with diabetes
What is A1c?
The A1c, also known as hemoglobin A1c, HbA1c, glycated hemoglobin, or glycohemoglobin, is a blood test that measures your average blood sugar over the last 2 to 3 months.
It’s not an “even average,” but rather a weighted average, where your blood sugar levels over the last few weeks count a little more than your blood sugar levels from 2 to 3 months ago.
According to the National Institute of Diabetes & Digestive & Kidney Diseases (NIDDK):
“The A1c test is based on the attachment of glucose to hemoglobin, the protein in red blood cells that carries oxygen.
In the body, red blood cells are constantly forming and dying, but typically they live for about three months. Thus, the A1c test reflects the average of a person’s blood glucose levels over the past three months.
The A1c test result is reported as a percentage. The higher the percentage, the higher a person’s blood glucose levels have been. A normal A1c level is below 5.7 percent.”
NIDDK
It’s important to note here that the term “normal A1c level” in this context refers to people without diabetes. I will get back to what a “normal A1c level” is for people living with diabetes below.
How to test your A1c
Your doctor or endocrinologist should check your A1c regularly (typically every 3 to 6 months). The doctor simply pricks your finger and takes a tiny blood sample.
If the doctor’s office has an A1c kit, you should get your result before your consultation is over. (Some offices, however, will send a blood sample from the lab for processing.)
You can also buy home A1c kits (no prescription required) and do the test yourself. Home A1c kits can be useful if you go for more than 3 months between doctor visits and want to keep an eye on how your A1c is trending.
The home kits are generally accurate within plus/minus 0.5 percentage points, which is more than good enough to give you a trustworthy result.
The downside of the home kits is that they require a larger amount of blood (generally, several large drops) than a regular blood sugar check, and if you don’t apply enough blood, you’ll get an error message and will have lost an A1c test strip.
You can find home test kits on Amazon and in some pharmacies. Be sure that your home A1c kit is used prior to the expiration date.
Read more in: How to Measure Your A1c at Home.
Why you should care about your A1c
Multiple significant studies have shown that high average blood sugars increase the risk of diabetes-related complications. Lowering your A1c to the recommended range will reduce the risk of diabetes-related complications.
According to the landmark Diabetes Control and Complications Trial (DCCT) and the follow-up study called the Epidemiology of Diabetes Interventions and Complications (EDIC), in people with diabetes who used intensive treatment to keep their A1c at the target level:
- Eye disease risk was reduced by 76 percent
- Kidney disease risk was reduced by 50 percent
- Nerve disease risk was reduced by 60 percent
- Any cardiovascular disease event risk was reduced by 42 percent
- Nonfatal heart attack, stroke, or risk of death from cardiovascular causes was reduced by 57 percent
Achieving an A1c in the recommended range is, therefore, one of the most important things you can do to improve your long-term health when you live with diabetes.
In some cases, lowering your A1c too much may not be a good idea if it means that you increase how often you experience hypoglycemia (low blood sugar).
I will explain why a measure known as “time-in-range” (TIR) is just as important as a low A1c later in this guide.
How to lower your A1c
Now that you have a thorough understanding of A1c, as well as why looking at your A1c in isolation isn’t optimal, the obvious question is:
How do you lower your A1c while improving or maintaining your time-in-range?
I will cover what, in my experience, are the four most important things you can do below, but it’s always recommended that you start by having a conversation with your medical team before making changes to your diabetes management.
Identify the main “pain points”
Whether you are largely self-managing your diabetes or working closely with your medical team, the first step should always be to try to identify the main “pain points,” or reasons why your A1c is higher than you’d like. The only real way of doing this is by tracking your blood sugars very closely.
If you wear a continuous glucose monitor (CGM), you can look at your 7-day, 30-day, and 90-day blood sugar data to see if you can spot any trends.
For example, you might find that you are running high from 1 a.m. to 5 a.m. every night, every morning (as in the dawn phenomenon, an early-morning increase in glucose level), or every day after meals. Or perhaps you always go low after exercise. We all have different blood sugar patterns.
It’s also very possible that you simply are running your blood sugar a little too high all the time and could benefit from adjusting your diabetes medication.
Identifying patterns like that makes it possible to pinpoint areas of potential improvement so you can start making a plan for how to limit your high and low blood sugars.
If you rely on manual blood sugar monitoring, it’s a little trickier since most people don’t monitor every five minutes. In this case, you might try increasing how often you check for a while, and maybe even checking during the night if you wake up anyway.
Most meters allow you to download data to your computer, or you can upload these data to one of various app-based platforms. This can help you see the data in a more cohesive way so you can start looking for trends.
Create a plan for your diabetes management
Now that you have a better idea of what your “pain points” are, you can start making changes to your diabetes management.
Your doctor may suggest a different medication regime. For example, some people are prescribed metformin to help with the dawn phenomenon. Others may need adjustments to insulin dosing or other medications.
If you’re using insulin and consistently have high blood sugars in the morning, getting your blood sugar fluctuations and A1c down might be as simple as adjusting your nighttime basal (background) insulin.
Or, if you run high every day after meals, your insulin-to-carb ratio might be off, and adjusting that could be what sets you on a path toward a lower A1c. Until you collect the data and do the analysis, you have no way of knowing this.
I want to make an important point here: increasing your diabetes medication is not a sign of failure. It’s often the best (and sometimes only) way to manage your blood sugar and bring down your A1c.
I adjust my insulin up and down all the time when I change my diet or exercise routine. The ability to adjust your medication is an important tool in your diabetes toolbox and something you should always discuss with your medical team.
Understand nutrition and adjust your diet
What you choose to eat and drink can have a major impact on your waistline, mood, and well-being, as well as your blood sugar levels.
All macronutrients (carbohydrates, proteins, and fats) can affect your blood sugar to some degree, so developing a good understanding of how they affect your blood sugar will enable you to be proactive and prevent blood sugar swings.
Carbohydrates (carbs)
Carbohydrates have the greatest impact on your blood sugar, which is why many people with diabetes can benefit from following a lower-carb diet. The fewer carbs you eat, the less insulin you need to take, which makes diabetes management easier.
However, you don’t have to follow a low-carb diet if it doesn’t work for you — physically or mentally.
As I wrote in my piece about which diet is best for people with diabetes, it is very possible to have great blood sugar management on a medium- (or even high-) carb diet, as long as you experiment, take notes, and learn to take the right amounts of insulin for the carbs you are eating.
It is very important to realize that we all react differently to carbs, so you have to find the diet and foods that are right for you.
As an example, people react very differently to carbs like oats or sweet potatoes. Some people can eat oats with only a small increase in blood sugar, while others see a quick spike.
By simply knowing this, people having difficulties with a certain type of carb can choose to reduce their consumption or cut it out of their diet altogether.
Protein and fats
While carbs affect blood sugar most significantly, protein and fat also have an impact. Some, like Dr. Sheri Colberg, PhD, one of the world’s leading voices on diabetes and exercise, think that only looking at carbs when estimating blood sugar impact (and dosing insulin) is an outdated and inefficient way to pursue diabetes management.
In the opinion of some experts, you should focus more on total calories (read more about calorie counting and diabetes here).
The key thing to be aware of is that when protein and especially fat are consumed with carbohydrates, the energy from the meal will be released more slowly, which means that your blood sugars will be impacted more slowly as well.
While I don’t believe your diabetes management should completely dictate how you live your life and which diet you choose to follow, it can be worth evaluating which food choices make life easier for you.
By making a conscious choice of which type of nutrition plan to follow (the majority of the time), you can more easily establish healthy habits that will benefit not only your overall health but also your daily blood sugar levels, and thereby your A1c.
Increase activity (exercise)
While exercise is essential for building and maintaining good health and improving insulin sensitivity, it can be a double-edged sword if it constantly throws your blood sugars for a loop. Not only is that very frustrating, scary, and annoying, but it can also affect your A1c and time-in-range.
The key is to understand how different types of exercise affect your blood sugar levels and, if you use insulin, to learn your formula for balancing insulin and food around workouts.
Cardio
Cardio, such as brisk walking, jogging, swimming, biking, or dancing, are all excellent types of exercise. As little as 20 to 30 minutes a day can make a significant difference when it comes to improving insulin resistance and managing blood sugar levels.
Not only does exercise reduce blood glucose during exercise, but it also improves your insulin sensitivity for hours after your workout, meaning that you need less insulin.
If you treat your diabetes with insulin, you will have to manage your insulin levels so you don’t experience exercise-induced hypoglycemia. This comes down to reducing your insulin significantly or consuming carbs before your workout.
For many people, it may not be necessary to “carb up” to do up to 60 minutes of steady-state cardio, but there can be situations in which reducing insulin before exercise can’t be done, so additional carbohydrates must be consumed.
And it’s also important to remember that different people react differently based on a variety of factors, such as insulin sensitivity, timing of their last insulin dose, and fitness levels, so this may not be the case for you.
Resistance training
Adding resistance training to your daily routine, such as free weights, weight machines, resistance bands, or bodyweight exercises, can be instrumental in increasing your insulin sensitivity and lowering your A1c.
Whereas cardio will lower blood sugar during exercise and potentially up to about 48 hours after exercise, resistance training can increase insulin sensitivity for much longer.
This is because muscles work as little “glucose tanks” and you’ll store more glucose in your muscles rather than sending it directly to your bloodstream. The more muscles you have, the better your insulin sensitivity.
Just be aware that some people will see a temporary increase in blood sugars during intense resistance training, rather than a decrease.
The reason for the increase in blood sugar is that the improved insulin sensitivity from exercising is surpassed by your body’s increased glucose production from the adrenaline released by the activity.
This adrenaline causes your liver to break down glycogen to create glucose, and your body is producing the glucose faster than you can use it.
For a detailed guide, read: How Resistance Training Affects Your Blood Sugar.
The shorter-term effects aside, because resistance training is so effective at increasing your insulin sensitivity, it’s a great way to lower your blood sugar and A1c consistently.
If you exercise regularly, the effect of exercising overlaps from one workout to the next, and you essentially achieve a permanent increase in insulin sensitivity. (Be sure to work with your healthcare team to adjust your treatment regimen to avoid lows from your improved insulin sensitivity.)
Maintain a healthy weight
If you are overweight, losing as little as 5 to 10 percent of your weight can help with various health markers, including A1c levels.
In one study, people with type 2 diabetes who lost this amount of weight reduced their A1c by an average of 0.5 percent.
How quickly can you lower your A1c?
Since the A1c test shows your glucose over the previous 2 to 3 months, it will take at least a few weeks of consistent dietary and exercise changes to see the results reflected in your A1c level.
The exact timeframe will vary based on individual factors such as the intensity of the changes and how your body responds.
(This is simply due to the long-term nature of the test — the improvements will reflect in your glucose much sooner.)
In this video, I explain how I lowered my A1c in 30 days by following five simple steps:
Why you shouldn’t lower your A1c too quickly
It can be a good idea to approach lowering your A1c with a bit of caution. Just as crash dieting isn’t healthy, there can be some serious health risks associated with lowering your A1c too quickly.
I turned to Dr. Anne Peters, MD, Director of the USC Clinical Diabetes Program, and Professor of Clinical Medicine Keck School of Medicine of USC for an explanation:
“If you lower your A1c too quickly, many bad things can happen.
First, weight gain and total body swelling. Next, it can cause bleeding in the retina (back of the eyes) which can lead to blindness, and third, it can cause painful neuropathy [nerve damage] that never goes away.
It’s slightly different for newly diagnosed patients, but, in general, no one should try to go from an A1c of 10 percent to 6 percent quickly. Take slow steps. Wanting to get to a ‘low’ number very fast only causes harm.
Diabetes is a long-term disease, so slow steps to establish new habits that can last a lifetime are the way to go. Anything too sudden, and the body reacts badly.”
Dr. Anne Peters
Can your A1c be too low?
As described above, the answer to this question depends almost entirely on how often you experience hypoglycemia. If you (almost) never experience hypoglycemia and your A1c is at target, this would suggest that your diabetes management is effective.
However, this doesn’t mean an extremely low A1c is always safe or desirable. Each person’s ideal A1c level can vary, and factors such as their risk of hypoglycemia unawareness, how long they have had diabetes, age, and overall health need to be considered.
If you often experience hypoglycemia, that will result in an “artificially” low A1c reading because your hypoglycemia events are lowering your blood sugar average.
In that case, focusing on increasing time-in-range is much more important than further lowering your A1c. In fact, you may even benefit from a slightly higher A1c with fewer blood sugar fluctuations.
It’s also important to note that lowering your A1c below the generally recommended range of 6.0 to 7.0 percent hasn’t been proven to provide any health benefits. Therefore, a very low A1c shouldn’t be a goal in itself.
What is a good A1c target?
Now that you have your A1c number, let’s look at what that number actually tells you. The American Diabetes Association has established the following guidelines:
| A1c Level | What It Means |
| Less than 5.7 percent | Normal (minimal risk for type 2 diabetes) |
| 5.7 percent to 6.4 percent | “Prediabetes,” meaning at risk for developing type 2 diabetes |
| 6.5 percent or greater | Diagnosed diabetes |
This does NOT mean that you need an A1c of less than 5.7% if you’re living with diabetes. It means that if you do NOT live with diabetes, your A1c is expected to be below 5.7%.
There are different recommendations for what an appropriate A1c is for people living with diabetes.
I had a chance to ask Dr. Peters, as well as Gary Scheiner, MS, CDCES, owner and Clinical Director of Integrated Diabetes Services and author of Think Like a Pancreas, what their perspectives are on a good A1c target:
Dr. Peters:
“The A1c target should be whatever is best given the person’s clinical situation.
For athletes, too many lows can limit performance, for someone who is pregnant it should be less than 6.0 percent, for an older person the target should be higher.
I generally think an A1c target of 6.0 to 7.0 percent is ideal and data shows that going below 7.0 percent has fairly little impact on complications.
Basically, I’d rather see someone with an A1c of 6.9 percent and low blood sugar variability than an A1c of 6.2 percent with lots of variability.”
Dr. Anne Peters
Scheiner:
“A1c goals should be individualized based on the individual capabilities, risks, and prior experiences.
For example, we generally aim for very tight A1c levels during pregnancy and more conservative targets in young children and the elderly.
Someone with significant hypoglycemia unawareness and a history of severe lows should target a higher A1c than someone who can detect and manage their lows more effectively.
And certainly, someone who has been running A1cs in double digits for quite some time should not be targeting an A1c of 6.0 percent … better to set modest, realistic, achievable goals.”
Gary Scheiner
Read more about A1c in: What is a “Normal” HbA1c? and What is a Dangerous Level of A1c?
In their Standards of Care in Diabetes — 2024, the American Diabetes Association recommends an A1c target of below 7.0 percent for adults living with diabetes.
An A1c of 7.0 percent roughly translates to an average blood sugar of 154 mg/dL (8.6 mmol/L) as you can see from this conversion chart (eAG stands for “estimated average glucose”).
| A1c | eAG (mg/dL) | eAG (mmoL) |
| 5 percent | 97 | 5.4 |
| 6 percent | 126 | 7.0 |
| 7 percent | 154 | 8.6 |
| 8 percent | 183 | 10.2 |
| 9 percent | 212 | 11.8 |
| 10 percent | 240 | 13.3 |
| 11 percent | 269 | 14.9 |
| 12 percent | 298 | 16.5 |
| 13 percent | 326 | 18.1 |
| 14 percent | 355 | 19.7 |
Learn more about converting A1c to average glucose levels in: How to Translate Your A1c to a Blood Sugar Level.
A1c vs. time-in-range
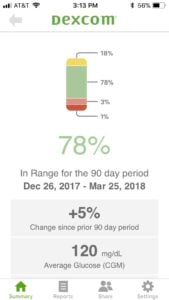
A1c has long been considered the best measure of diabetes management because it was the most accurate tool for observing long-term blood sugar trends. This has changed with the introduction of continuous glucose monitoring (CGM).
By using a CGM, you can now get a very accurate picture of not only your average blood sugar, but your blood sugar fluctuations as well.
This makes it possible to track another key component of diabetes management: time-in-range.
Time-in-range refers to the percentage of time during which your blood sugar is within a specific range. To see why time-in-range is important, take a look at the three lines in the graph below.
All three lines show an average blood sugar of about 154 mg/dL (8.6 mmol/L, which equates to an estimated average A1c of about 7.0 percent) but with very different fluctuations. I think we would all prefer our blood sugar to follow line 3 rather than line 1.
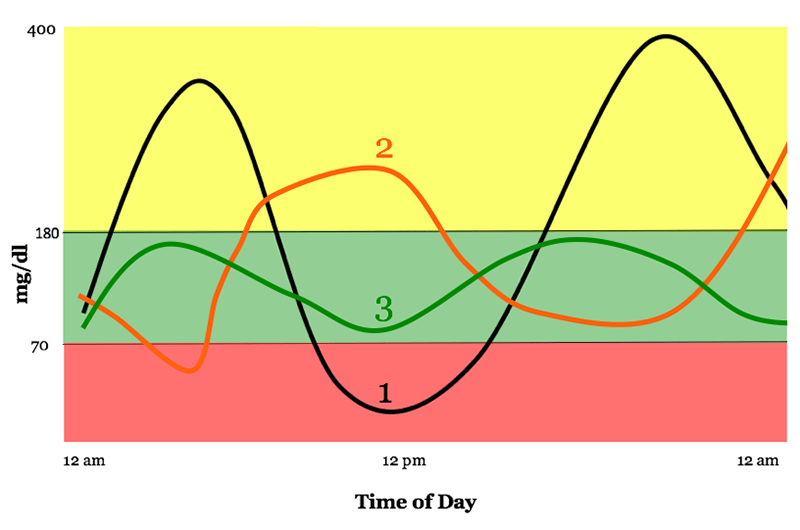
Graph used with permission from diaTribe.
Some guidelines state that your blood sugar range should be set to 70 to 180 mg/dL (3.9 to 10 mmol/L), but you may find that to be too wide or narrow of a range for you.
In this interview with several diabetes experts, most recommend that you spend less than 3 percent of the time below 70 mg/dL (3.9 mmol/L) and less than 1 percent of the time below 54 mg/dL (3 mmol/L). However, they also agree that the actual time spent in range needs to be individualized.
On average, the experts didn’t expect the general diabetes population to be in range more than 50 percent of the time at most, so talking about incremental improvement makes more sense than setting a fixed number.
How to measure time-in-range
If you wear a CGM, your time-in-range metrics should be listed when you download your data (as in the example from a Dexcom CGM below).
Some CGM devices offer alerts when glucose levels are predicted to enter or leave the target range, which can allow users to respond proactively and spend more time in range.
(Click to expand.)
If you don’t use a CGM, all you can do is look at your manual blood sugar measurements and pay attention to the amount of high and low blood sugar readings outside of your target range.
What’s an acceptable high and low is something you have to discuss with your medical team.
What is more important: a low A1c or a high time-in-range?
Ideally, you’d have an A1c below 7.0 percent accompanied by low blood sugar variability (high time-in-range). A good general guideline is:
- The higher your A1c, the more important it is to focus on getting it down.
- The lower your A1c, the more important time-in-range becomes.
If your A1c is below 6.0 to 7.0 percent, focusing on increasing your time-in-range will probably have a larger positive health impact than lowering your A1c further.
So, is A1c the best way to gauge whether your diabetes management is on track? Not necessarily, but to quote Scheiner:
“I’ve never been a huge fan of using A1c to gauge the ‘quality’ of a person’s glucose control, simply because it represents an average … and an average can reflect lots of highs and lows rather than time spent within one’s target range.
However, it’s not something we can ignore either since there is a correlation between A1c and the risk of long-term complications.”
Gary Scheiner
Final thoughts: My perspective on A1c as a person living with diabetes
I have a very ambivalent relationship with my A1c myself. I’ve been living with type 1 diabetes for over 20 years, and my A1c is not something I think about in my daily life.
However, every 3-6 months, when I see my endo, I get a little anxious because receiving your A1c can feel a lot like getting your diabetes report card.
And, quite honestly, that’s really silly. My A1c number doesn’t reflect what’s been going on in my life for the last 3 months. It doesn’t tell me how much effort I’ve put into managing my diabetes, and it does not define me as a person. It’s a good source of information, nothing more.
Still, we tend to look at it and judge, good or bad, how we’ve done with our diabetes management. But we really shouldn’t!
That doesn’t mean that I think we shouldn’t get our A1c checked. I absolutely think we should, but we also need to understand what it means as well as why we should look beyond the A1c number. I hope this guide has given you the knowledge and tools to do so.






Rob
im 39 i get a physical every year and in 12 months time I went from non diabetic to type 2 with 244 glucose and 11.1 A1c. I was thin most of my life and gained weight after 30 5″8 and 225 6 weeks ago. I started doing keto and im down to 199 with bloodwork in a few days. The odd thing is i didnt feel sick before the diagnosis and now after dieting i feel tired and irritable. I do not drink, smoke, or do drugs so food is my one vice. I have no idea how i am suppose to live life hungry 24/7 and completely miserable. What do i do?
Christel Oerum
If you feel that way while eating a keto diet, I’m not sure that’s the right option for you. There’s more to health than losing weight. I would ask your doctor for a referral to a Registered Dietitian (RD) to help you build a diet that works for you. The thing is, there’s no ONE way of living well with diabetes, and it can take a few tries to find what’s right for you
T Sams
I was doing faithful Keto and my A1c was 9.5 and my average glucose numbers were 173. I decided to try a vegan diet and within two months my A1c was at 6.1. I understand that is a rather fast drop, but my A1c also moved up rapidly. The only problem of late is a bit of hypoglycemia, but what I have tried to do is take my diabetes medicine earlier and per doctor’s orders cut back on some meds and check my numbers before I go to bed. If I can keep my numbers in that 140 – 160 range at night, I tend to wake up with a fasting glucose reading of 70.
The next step is to try a Dexacon reader that I can easily check my number throughout the day and make sound eating choices. I am trying to close the spread between the fast and after I eat.
There is also an excellent UK medical study where the patients stuck to an 823 – 850 calorie diet and results were remarkable. You can find the study here: https://evidence.nihr.ac.uk/alert/type-2-diabetes-can-be-reversed-with-a-low-calorie-diet/
genoveva castillo
hi,
I have my a1c 12 , and my sugar levels of 300 i want to do changes im afaid of what can happened to me, i read the comments here and im very surprised of all the things they say
thank you
Christel Oerum
With blood sugars that high I’d recommend you reach out to your doctor as soon as possible and discuss a treatment plan. If you’re already using insulin the doctor can help guide you on how to adjust it to get your blood sugars down
Martha
Love your post ? on helping others with great tool to make a healthy change in our lives thanks
Dianne
I am a type 2 diabetic, caused by cysts on my pancreas, one at the duct. 3 months ago
My A1C was 7.0, I am on 5 (500 mg) a day. The day after I got my A1C result, I started Keto and walking I walk 60 minutes a day split in two, and I do strength training after each walk 7 days a week. Yesterday was my bloodwork since I changed my diet and started seriously exercising for 3 months, and I was shocked it only came down to 6.8 . I did have to up my carbs a bit during those last 2 months as I kept losing weight and have gone down to a below normal weight for myself, and I am struggling putting on weight as i am still careful with my carb intake. I eat 160 to 180 grams a day.I really had hoped my A1C would have been lower after the hard work of diet change and walking and strength training during those 3 months. Any suggestions on what mistake I am making?
Christel Oerum
Sounds like you’re doing everything in your power. You might need to give it more time or have your medication adjusted. AS for your diet, I’d suggest working with a registered dietitian (RD) to help you achieve your goals and ensure that you stay healthy. One option is to look up Ben Tzeel, RD (https://www.yourdiabetesinsider.com/).
I’d also encourage you to read this article on reversing Type 2 diabetes (https://www.yourdiabetesinsider.com/)
Laurie Phillips
Why is it so hard to get a flat stomach as a diabetic? I am Type 2 since 2008 and on a 25 to50 net carb diet since I went of metformin which made my gastroparesis worst. My sugars are great and I have lost 8lbs since January. No change in stomach or bigger than before. How much exercise is good for this issue. I do walk 3 to 5’000 steps a day with walk and love to walk. Should I add exercises just for gut ? I used to run when I was younger but like hiking better since I am older almost 60.
Christel Oerum
I do see a fair amount of people living with diabetes who are very lean, so I’m starting to think that it has more to do with our body types than our diabetes. You’re already on the right path for weight loss, the stomach might just be the last to go. And remember, for weight loss, you have to think about your overall calorie balance so it’s not just about much you move but also how many calories you consume
Anil
First, thanks for such a well written blog, Christel.
I am one such example; lean, vegetarian, south Asian, mainly rice eater, non smoker, non alcoholic, etc. My type 2 diabetes baffles my doctors! They say it is very difficult to understand ?
Anyway, I recently started using CGM. It has been a boon. Now I exactly know how my body is reacting to the food I eat. All general guidelines and myths debunked for me. I am on my third monitor and exactly know how and when I need to take medication, and how food and stress affect my bg.
As for losing weight, even though I was high normal before, Jardiance with diet made me lose 15 pounds 2 years ago. But when pandemic hit and I started working from home, gained back the same in mid section ?.
Sitting at one place attending online meetings 8-9 hours a day is dangerous!
c
I am early 60s, normal weight, exercise a lot. the last few years, they have added the HbA1c test to my annual physical. my fasting blood sugar is always about 86 but my HbA1c is about 5.7… so they look at me cross eyed at the drs. This year I have decided no added sugar foods for 3 months- yeah, so much for my birthday and ice cream this summer. I actually do like cake now and then and dark chocolate but I do not drink any sugary drinks or eat fruit and I am a lacto ovo vegetarian. If my HbA1c is the same after 3 mos, I will not be happy. 🙁
Kathleen
I was taking off of Metformin. My doctor said it wasn’t worth it. Check with your doctor.
Jac
Spouse had numbers in the 300’s and highs in the 400’s and 500’s, around Thanksgiving/Christmas 2020. Had A1C test for over 2 years around 10-11. We decided to make drastic changes to eating habits and exercise. Went full carnivore(she was not a big meat eater), with some cheese as snacks, slowly started adding other things like healthy fats(nuts, avocados), beans. Got A1C tested again after about 1.5 months, A1C were down to 6.8. Will continue to work to get down under 5.7 as she continues to feel stronger and healthier. We gave up on endos, no longer felt they had her best interest in mind, sadly seemed like keeping her sick was better for their financial gains and seems like our own path is working well, we all know our bodies better than anyone else. Good luck to everyone on their journey.
Patricia Drier
I absolutely loved this article on! It has helped me understand more about A1c. Thank you!
Christel Oerum
Good, I’m glad to hear that
Inam
Hello mam
Iam 27 years old and person who always preferred healthy life style . I always tried to eat as healthy as i can. Workout is in my life from many years as i like going to gym . Coming to the point 15 days back i went with my sister to check her fasting sugar as she is pregnant I also thought to get my self tested. Shocking thing was my Fasting sugar was 262 and random after 2 hours of meal was 225 .. than i tested my HBA1C which was 10.9 … after this horrible result i made lot of changes as i reduced carbs from my diet and i added 30 minutes walk before bed and few fruits and aftr 15 days now my fasting is between 96 to 120 and random is between 125 to 150 .. what i want to ask is iam confused either iam diabetic or iam pre diabetic ? Should i visit doctor as many doctors recommend medicine is their any way that i can reverse it with diet and exercise ?
Christel Oerum
I’m so glad you chose to get tested! I would highly recommend you go see a doctor and get the appropriate blood work done. You could be pre-diabetic, have type 2, type 1, or LADA. THere’s no way to know without the right blood tests. Often adults are dismissed as pre-diabetic or having type 2 diabetes but it important to get tested for antibodies so that you know how to proceed. If you get diagnosed with type 1 or LADA you will be required to use insulin as they are autoimmune conditions. Below 2 links so you can read more about type 1 and LADA
https://diabetesstrong.com/category/diabetes/type-1/
https://diabetesstrong.com/lada-diabetes/